 |
 |
- Search
| Obstet Gynecol Sci > Volume 67(2); 2024 > Article |
|
Abstract
Objective
Geriatric patients requiring gynecological surgery is increasing worldwide. However, older patients are at higher risk of postoperative morbidity and mortality, particularly cardiopulmonary complications. Laparoscopic surgery is widely used as a minimally invasive method for reducing postoperative morbidities. We compared the outcomes of open and laparoscopic gynecologic surgeries in patients older than 55 years.
Methods
We included patients aged >55 years who underwent gynecological surgery at a single tertiary center between 2010 and 2020, excluding vaginal or ovarian cancer surgeries were excluded. Surgical outcomes were compared between the open surgery and laparoscopic groups, with age cutoff was set at 65 years for optimal discriminative power. We performed linear or logistic regression analyses to compare the surgical outcomes according to age and operation type.
Results
Among 2,983 patients, 28.6% underwent open surgery and 71.4% underwent laparoscopic surgery. Perioperative outcomes of laparoscopic surgery were better than those of open surgery in all groups. In both the open and laparoscopic surgery groups, the older patients showed worse overall surgical outcomes. However, age-related differences in perioperative outcomes were less severe in the laparoscopic group. In the linear regression analysis, the differences in estimated blood loss, transfusion, and hospital stay between the age groups were smaller in the laparoscopy group. Similar results were observed in cancer-only and benign-only cohorts.
With prolonged life expectancies owing to advances in medicine, the age of patients with gynecological diseases is increasing. Consequently, the number of geriatric patients requiring gynecological surgery is increasing [1,2]. Age is a well-known independent risk factor for perioperative morbidity and mortality [3-5]. Therefore, finding an optimal treatment for older patients is a pressing issue that requires a solution.
Recently, the number of laparoscopic gynecological surgeries has increased significantly for both benign and malignant conditions. Laparoscopy and minimally invasive surgery have become major trends, with studies consistently reporting improved perioperative outcomes with the laparoscopic approach compared with open surgery [6-8]. Given that older patients are vulnerable to surgery, the benefits of laparoscopy may be magnified in this population.
However, older patients are vulnerable to laparoscopy for several reasons, including longer operation time and the influence of pneumoperitoneum [4]. Anesthesiological studies have demonstrated that increased systemic carbon dioxide resulting from pneumoperitoneum can exert a burden on the heart and lungs, especially in patients with impaired cardiopulmonary function, which is common in older patients [9,10]. In contrast, there are reports showing the safety of laparoscopic surgery compared with open surgery in colorectal cancer patients, with a shorter hospital stay and reduced cardiopulmonary morbidity [11,12].
Previous studies have evaluated the safety and feasibility of laparoscopy in gynecological surgery for older patients [13-15]. However, the definition of ŌĆ£older patientsŌĆØ is arbitrary and varies between studies. In this study, we evaluated the safety of laparoscopic surgery in older patients with gynecological diseases. In addition, we compared age-related increases in surgical morbidity between open and laparoscopic surgery.
The study population included patients aged >55 years who underwent gynecologic surgery between 2010 to 2020 at a single tertiary center in the Republic of Korea. The list of patients and data was obtained from the clinical data warehouse, Data Analytics and Research Window for Integrated Knowledge, of the institution. The medical records of these patients were retrospectively reviewed. Approval from the Institutional Review Board (IRB) of Samsung Medical Center was obtained (No. 2022-03-102-001), and informed consent was waived by the IRB because this was a retrospective study.
Surgical indications included benign or malignant uterine and adnexal pathologies. Benign diseases included benign ovarian cysts (serous/mucinous cystadenoma, mature cystic teratoma, and endometriosis etc.), paratubal cysts, uterine myomas, adenomyosis, intraepithelial lesions of the uterine cervix, endometrial polyps, endometrial hyperplasia, or pelvic organ prolapse. Malignant diseases included endometrial cancer, cervical cancer, uterine sarcoma, vulvar cancer, and Krukenberg cancer of the ovaries. Surgeries for the staging or cytoreduction of ovarian cancer were excluded from the study. Surgery for biopsy was also excluded. The main surgical procedures included in this study were hysterectomies and salpingo-oophorectomies. Since our study population consisted of individuals aged 55 or older, all of whom were either in a menopausal or perimenopausal state. Consequently, ovarian cystectomy was not performed on any patient. Instead, risk-reducing salpingo-oophorectomy was performed in 52 patients, with one patient undergoing concurrent hysterectomy, and all surgeries were performed laparoscopically. The attending physician determined the surgical method at the time of treatment. The single-port approach, dual-port approach, conventional multiport laparoscopy, and robotic surgery were considered laparoscopic surgeries. Cases that were converted from the laparoscopic approach to the open approach during surgery were considered open surgeries. Patients who underwent surgery via the vaginal approach were excluded. Fig. 1 shows the detailed selection process for the study population.
Patients were divided into two groups according to whether the surgical approach was laparoscopic or open. The patients were divided into younger and older groups according to whether they were above or below 65 years of age at the time of surgery. The age cutoff was set at 65 years, which showed the most statistically significant difference between the younger and older groups. Preoperative variables, including age, body mass index, and American Society of Anesthesiologists physical status score (ASA score) were investigated by reviewing medical records. Surgical outcomes, including estimated blood loss (EBL), transfusion, operation time, length of hospital stay, hospital readmission within 6 weeks after surgery, and mortality within 6 months after surgery, were also evaluated.
The data obtained were analyzed using R software version 4.0.4 (R Institute for Statistical Computing, Vienna, Austria). Statistical analyses were performed using the Student t-test or Mann-Whitney U-test for continuous data and the Pearson chi-squared test or FisherŌĆÖs exact test for categorical data. Linear regression or logistic regression analyses were performed to compare surgical outcomes according to age and operation type. Skewed data were analyzed using a variable-root transformation. Values of P<0.05 were considered statistically significant.
A total of 2,983 patients were included in this study. Among them, 28.6% (n=853) underwent open surgery and 71.4% (n=2,130) underwent laparoscopic surgery. After dividing the patients into younger and older groups, with 65 years as the base, 68.3% (n=2,036) were younger and 31.7% (n=947) were older. The baseline characteristics of the patients are summarized in Table 1. The mean age of the patients in the older group that were in the open surgery group was 71.4 and 70.5 for the laparoscopy group (P=0.013). Laparotomy was preferred in patients with ASA scores of 3 and 4. There were more cases of malignant disease in those who underwent open surgery and more cases of benign disease in those who underwent laparoscopic surgery in both the older and younger groups.
We compared the outcomes of open and laparoscopic surgeries between the two age groups. In both the younger and older groups, patients who underwent laparoscopic surgery showed better surgical outcomes than those who underwent open surgery (Table 2). Particularly, in the older group, the perioperative outcomes of laparoscopic surgery were better than those of open surgery (EBL, 336.7 vs. 100.0 mL, P<0.001; transfusion, 1.4 vs. 0.1 pints, P<0.001; operation time, 209.3 vs. 141.4 minutes, P<0.001; hospital stay, 11.6 vs. 5.4 days, P<0.001), and similar better outcomes with laparoscopic surgery were observed in the younger group. The readmission rate in 6 weeks was also lower in the laparoscopy group than in the open surgery group in both age groups (age <65 years, 16.5% vs. 3.3%, P<0.001; age Ōēź65 years, 18.2% vs. 4.1%, P<0.001). Mortality at 6 months after surgery did not differ between the surgical approaches in either age group.
Fig. 2 shows a comparison of surgical outcomes between the younger and older groups according to the surgery type. In the open surgery group, patients older than 65 years had worse overall outcomes. The operation time and readmission rate at 6 weeks did not show any difference between the young and old groups. In the laparoscopy group, older patients showed a lower EBL than younger patients (114 vs. 100 mL, P=0.016). Patients older than 65 years had a longer operation time and duration of hospital stay (operation time, 114 vs. 141 minutes, P=0.389; hospital stay, 5.1 vs. 5.4 days, P=0.069) and higher rates of readmission and death (readmission in 6 weeks, 3.3% vs. 4.1%, P=0.433; death in 6 months: 9.4% vs. 16.7%, P=0.724) than younger patients, but the difference was not statistically significant.
Linear regression analysis was performed to simultaneously evaluate the effects of age and surgical approach on surgical outcomes. The differences in EBL, transfusion, and duration of hospital stay between the younger and older groups were smaller in the laparoscopy group than in the open surgery group with a statistical significance (EBL, P=0.040; transfusion, P<0.001; hospital stay, P=0.003). Logistic regression analysis was also done to compare the age-related deterioration rates of readmission and death according to the surgical approach, but it did not show statistical significance (readmission at 6 weeks, P=0.734; death at 6 months, P=0.775).
Since malignant disease surgery is more extensive and takes longer than benign disease surgery, surgical outcomes were compared between patients with cancer. The results showed better surgical outcomes in patients who underwent laparoscopic surgery than in those who underwent open surgery in both the younger and older groups (Table 3). In the cancer cohort, the differences in EBL, transfusion, and duration of hospital stay between the younger and older groups were also smaller in the laparoscopy group than in the open surgery group with statistical significance (EBL, P=0.027; transfusion, P=0.001; hospital stay, P=0.033; Fig. 3).
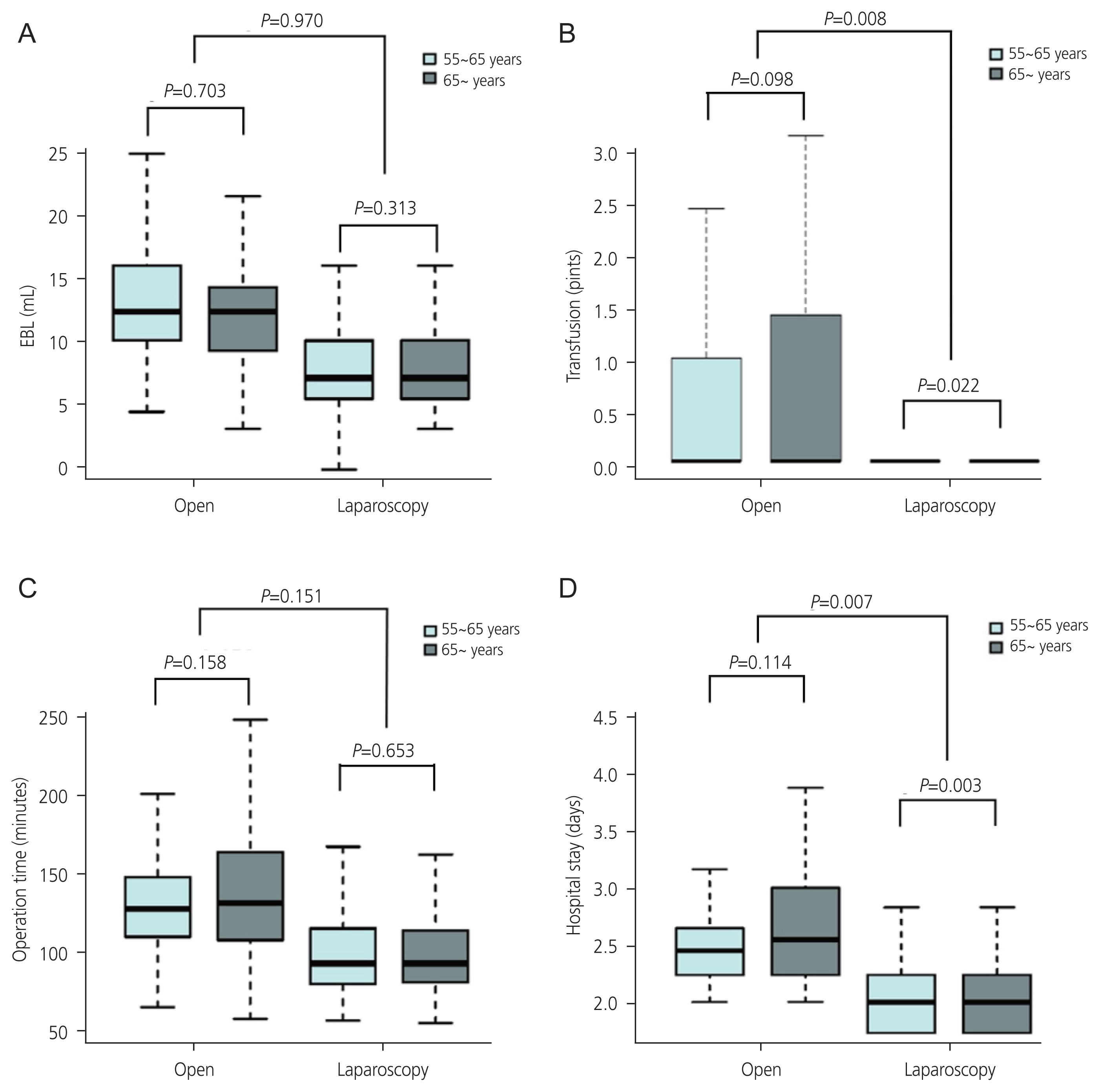
We also compared the surgical outcomes between patients with benign diseases. Similar to the cancer cohort, the results showed better surgical outcomes in patients who underwent laparoscopic surgery than in those who underwent open surgery in both younger and older groups (Table 4). In the benign disease cohort, the differences in transfusion and duration of hospital stay between the younger and older groups were smaller in the laparoscopy group than those in the open surgery group with statistical significance (transfusion, P=0.008; hospital stay, P=0.007; Fig. 4).
Older patients have poor perioperative outcomes across multiple fields, with an increased risk of postoperative complications, medical complications, and mortality [16-18]. Many studies have demonstrated that laparoscopic gynecological surgeries are safe in older patients, with fewer side effects and better perioperative outcomes than open surgery [6-8,19]. This study showed that perioperative morbidity, which increases with age, can be reduced by using laparoscopy as a surgical method. Surgical outcomes were significantly worse in older patients in the open surgery group; however, the differences were not significant between the age groups in the laparoscopy group. Similar results were obtained when comparing patients with malignant diseases.
While it is evident from previous studies and our findings that open surgery may lead to less favorable outcomes than laparoscopic surgery, it is crucial to highlight noteworthy observations. Specifically, when we focused on cases involving the same type of surgery, there appeared to be less significant age-related deterioration in laparoscopic procedures than in open surgery. This suggests that laparoscopy may play a substantial role in mitigating the potential impact of advanced age on surgical outcomes. This finding underscores the importance of considering the surgical approach in the context of age and may have implications for optimizing treatment strategies in geriatric patients undergoing gynecologic surgery.
As the number of older patients increases, the need for surgery with reduced postoperative morbidity also increases. Pneumoperitoneum is an essential part of laparoscopic surgery, and there are concerns as to whether increased intra-abdominal pressure is safe for older patients, especially those with significant comorbidities [4,20-22]. Consequently, studies have been conducted on the safety and benefits of laparoscopic surgery in older patients. The LACC trial revealed lower rates of disease-free survival and overall survival after minimally invasive radical hysterectomy than after open abdominal radical hysterectomy for early-stage cervical cancer [23]. In the LAP2 trial, laparoscopic surgical staging showed better perioperative and postoperative morbidity rates than open surgery [6]. Bishop et al. [24], compared laparoscopic approach and open surgery for surgical staging with patients of early-stage uterine cancer, aged 60 years or older. The findings indicated that open staging surgery was more associated with postoperative complications, such as longer hospital stays, ileus, pneumonia, deep vein thrombosis, and arrhythmia [24]. Ciavattini et al. [13] also proved that gynecologic laparoscopy is feasible and safe in older patients, regardless of medical comorbidities. However, some studies have compared the safety of minimally invasive surgery between younger and older patients [24-26]. Unlike previous studies, our study has the advantage of simultaneously considering and analyzing two variables: age and surgical method.
Although many previous studies have highlighted the safety of laparoscopic surgery in older patients, it is essential to not disregard the potential impact of the disease itself, as cancer can act as a risk factor for patient deterioration, increased thrombosis risk, and other adverse effects on their condition. Therefore, we compared the surgical outcomes between open and laparoscopic surgeries by age group with only cancer and benign disease (Tables 3, 4), and similar results were found in each group. In addition, when considering the impact of cancer, it is important to account for potential differences in prognosis that may arise when patients undergo the same surgery but have different diagnoses (benign vs. cancerous).
Although there are different ways to classify a population, the definition of ŌĆ£older adultsŌĆØ varies from study to study. Some authors consider older age to be over 65 years, whereas others insist on more limited criteria, such as those older than 70 or 75 years [27-29]. Some studies have classified older adults aged 65-74 years as youngest-old, those aged 75-84 years as middle-old, and those aged over 85 years as oldest-old [30,31]. In this study, the reference point with the largest difference in perioperative outcomes was set as the standard for older patients through statistical analysis. These data can serve as a scientific basis for defining the older population (>65 years old).
This study had some limitations. First, this study was mainly based on medical charts, and its retrospective nature may have caused information bias. Specific surgery-related complications have not been investigated. Second, stratification analysis was not performed on very old age groups, such as 75 and 80 years old, since the number of those patients was too small in our cohort. Third, with the recent active introduction of robotic surgery, a comparison of the performances of robotic surgery is necessary. Fourth, our study did not specifically examine tumor staging. However, a greater tumor burden may increase the likelihood of opting for open surgery, with potential repercussions on surgical outcomes. As emphasized earlier, our primary objective was to underscore the disparities attributable to age rather than conducting a direct head-to-head comparison of outcomes between open and laparoscopic approaches. It is important to acknowledge that the tumor stage may have a significant influence on the choice of surgical approach and subsequent outcomes. This underscores the potential value of conducting further investigations on the interplay between tumor characteristics and surgical approaches.
In conclusion, adverse surgical outcomes in older patients were reduced by laparoscopic surgery. Therefore, laparoscopic surgery offers more advantages and is safer than open surgery in older patients over 65 years of age.
Notes
Fig.┬Ā1
Flowchart of patient selection. Patient selection was done by DARWIN-C (data analytics and research window for integrated knowledge-clinical data).
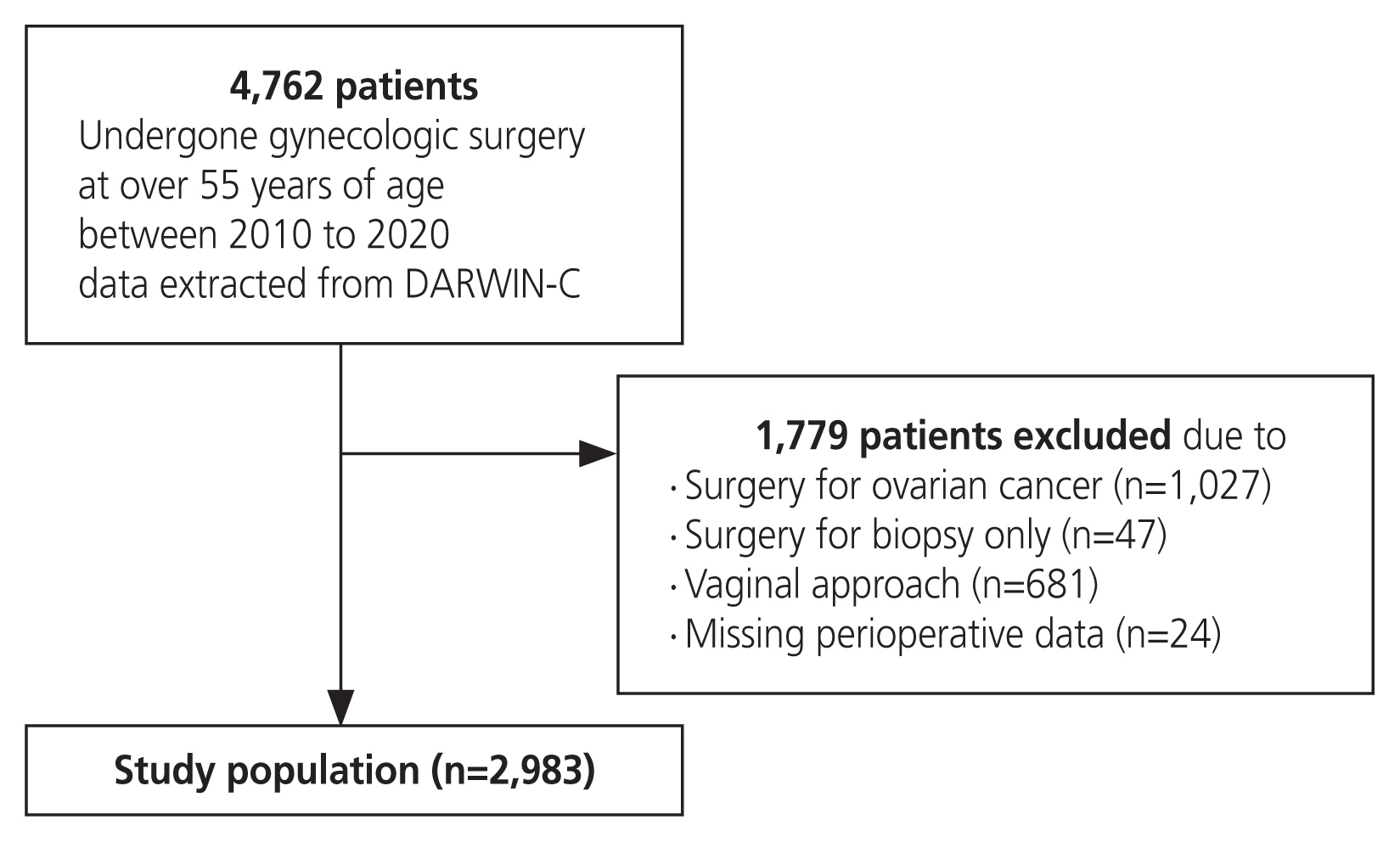
Fig.┬Ā2
Comparison of surgical outcomes between the age groups by surgical approach with linear regression analysis. (A) Comparison of EBL (mL) between age groups by surgical approach. (B) Comparison of transfusion (pints) between age groups by surgical approach. (C) Comparison of operation time (minutes) between age groups by surgical approach. (D) Comparison of hospital stay (days) between age groups by surgical approach. EBL, estimated blood loss.
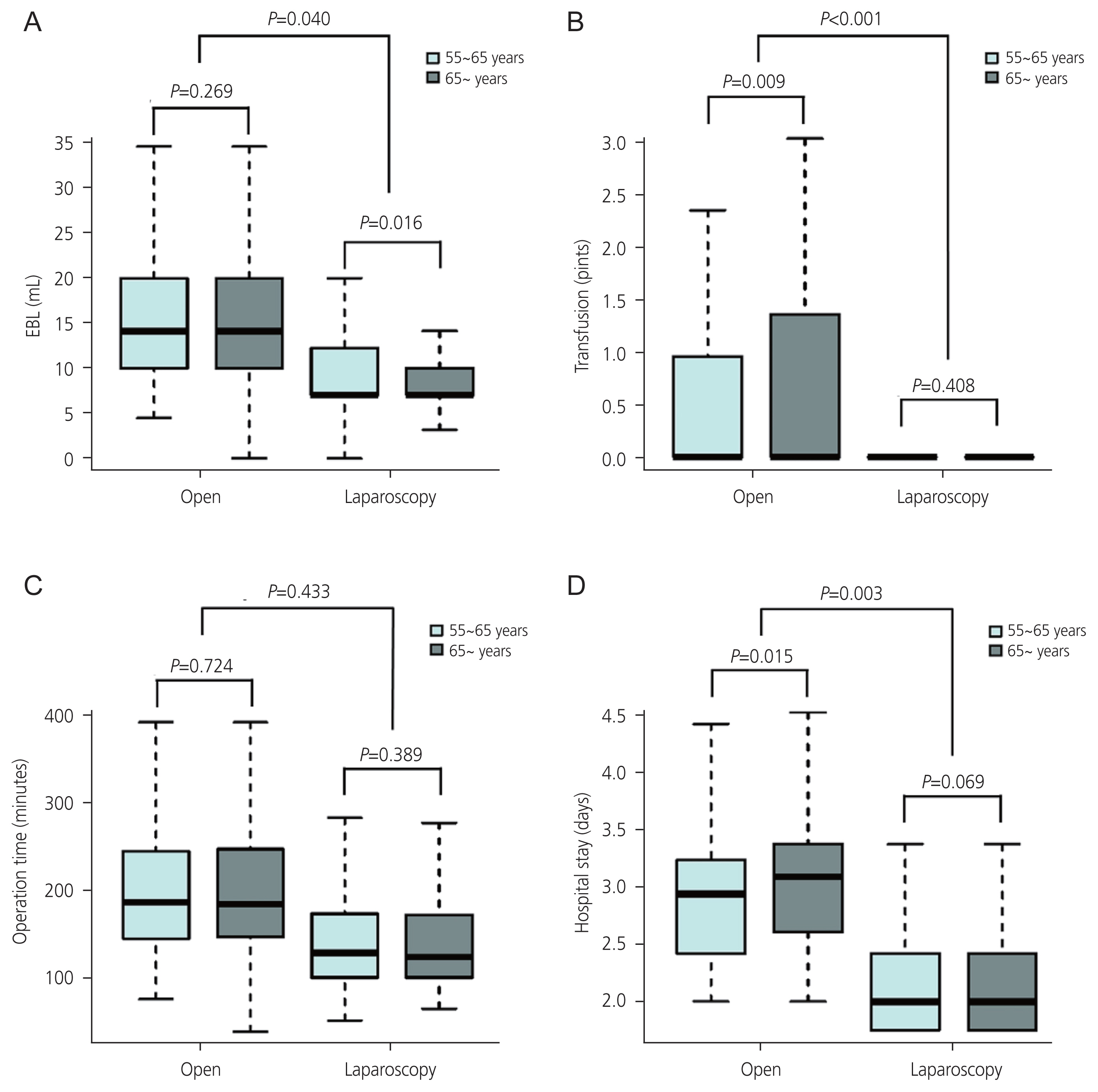
Fig.┬Ā3
Comparison of surgical outcomes between the age groups by surgical approach with linear regression analysis (cancer only). (A) Comparison of EBL (mL) between age groups by surgical approach (cancer only). (B) Comparison of transfusion (pints) between age groups by surgical approach (cancer only). (C) Comparison of operation time (minutes) between age groups by surgical approach (cancer only). (D) Comparison of hospital stay (days) between age groups by surgical approach (cancer only). EBL, estimated blood loss.
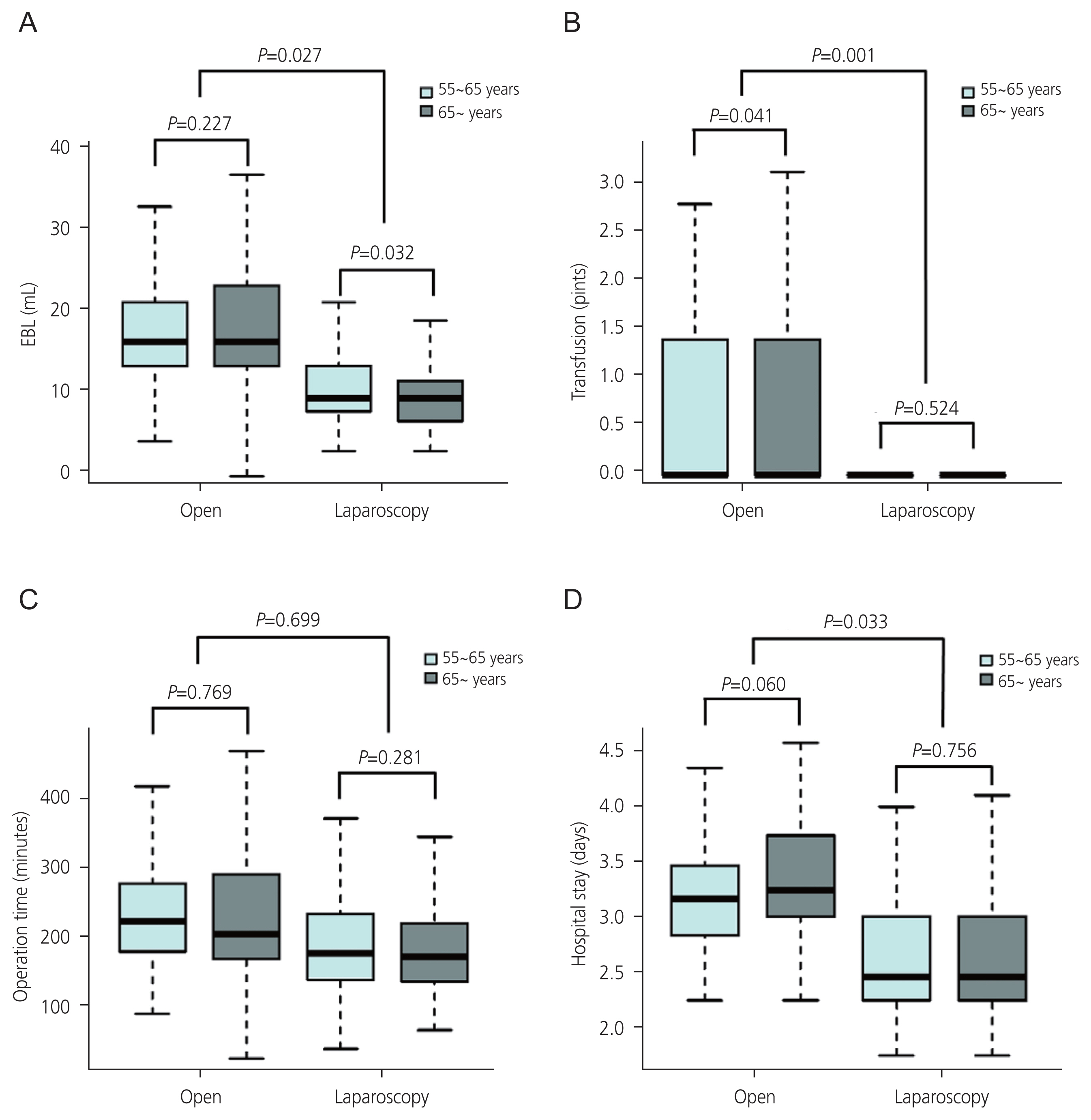
Fig.┬Ā4
Comparison of surgical outcomes between the age groups by surgical approach with linear regression analysis (benign only). (A) Comparison of EBL (mL) between age groups by surgical approach (benign only). (B) Comparison of transfusion (pints) between age groups by surgical approach (benign only). (C) Comparison of operation time (minutes) between age groups by surgical approach (benign only). (D) Comparison of hospital stay (days) between age groups by surgical approach (benign only). EBL, estimated blood loss.
Table┬Ā1
Baseline characteristics of the patients
Table┬Ā2
Comparison of surgical outcomes between open and laparoscopic surgeries by age group
Table┬Ā3
Comparison of surgical outcomes between open and laparoscopic surgeries by age group (cancer only)
Table┬Ā4
Comparison of surgical outcomes between open and laparoscopic surgeries by age group (benign only)
References
1. De Marzi P, Ottolina J, Mangili G, Rabaiotti E, Ferrari D, Vigan├▓ R, et al. Surgical treatment of elderly patients with endometrial cancer (Ōēź 65 years). J Geriatr Oncol 2013;4:368-73.


2. Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg 2006;203:865-77.


3. Hamel MB, Henderson WG, Khuri SF, Daley J. Surgical outcomes for patients aged 80 and older: morbidity and mortality from major noncardiac surgery. J Am Geriatr Soc 2005;53:424-9.


4. Cagli├Ā P, Tracia A, Buffone A, Amodeo L, Tracia L, Amodeo C, et al. Physiopathology and clinical considerations of laparoscopic surgery in the elderly. Int J Surg 2016;33(Suppl 1):S97-102.


5. Sultana CJ, Campbell JW, Pisanelli WS, Sivinski L, Rimm AA. Morbidity and mortality of incontinence surgery in elderly women: an analysis of Medicare data. Am J Obstet Gynecol 1997;176:344-8.


6. Walker JL, Piedmonte MR, Spirtos NM, Eisenkop SM, Schlaerth JB, Mannel RS, et al. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol 2009;27:5331-6.



7. Kolarsick PA, Sacchi M, Spinelli A, Wexner SD. Minimizing the impact of colorectal surgery in the older patient: the role of minimally invasive surgery in the geriatric population. Eur J Surg Oncol 2020;46:333-7.


8. Weber DM. Laparoscopic surgery: an excellent approach in elderly patients. Arch Surg 2003;138:1083-8.


9. Myre K, Buanes T, Smith G, Stokland O. Simultaneous hemodynamic and echocardiographic changes during abdominal gas insufflation. Surg Laparosc Endosc 1997;7:415-9.

10. OŌĆÖMalley C, Cunningham AJ. Physiologic changes during laparoscopy. Anesthesiol Clin North Am 2001;19:1-19.


11. Law WL, Chu KW, Tung PH. Laparoscopic colorectal resection: a safe option for elderly patients. J Am Coll Surg 2002;195:768-73.


12. Frasson M, Braga M, Vignali A, Zuliani W, Di Carlo V. Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum 2008;51:296-300.


13. Ciavattini A, Di Giuseppe J, Cecchi S, Tsiroglou D, Mancioli F, Stevenazzi G, et al. Gynecologic laparoscopy in patients aged 65 or more: feasibility and safety in the presence of increased comorbidity. Eur J Obstet Gynecol Reprod Biol 2014;175:49-53.


14. Buchweitz O, Matthias S, M├╝ller-Steinhardt M, Malik E. Laparoscopy in patients over 60 years old: a prospective, randomized evaluation of laparoscopic versus open adnexectomy. Am J Obstet Gynecol 2005;193:1364-8.


15. Suh DH, Kang S, Lim MC, Lee TS, Park JY, Kim TJ, et al. Management of the elderly patient with gynecologic cancer: report of the 2011 workshop in geriatric gynecologic oncology. Int J Gynecol Cancer 2012;22:161-9.


16. Hannan EL, Racz MJ, Walford G, Ryan TJ, Isom OW, Bennett E, et al. Predictors of readmission for complications of coronary artery bypass graft surgery. JAMA 2003;290:773-80.


17. Bentrem DJ, Cohen ME, Hynes DM, Ko CY, Bilimoria KY. Identification of specific quality improvement opportunities for the elderly undergoing gastrointestinal surgery. Arch Surg 2009;144:1013-20.


18. Massarweh NN, Legner VJ, Symons RG, McCormick WC, Flum DR. Impact of advancing age on abdominal surgical outcomes. Arch Surg 2009;144:1108-14.


19. Guy MS, Sheeder J, Behbakht K, Wright JD, Guntupalli SR. Comparative outcomes in older and younger women undergoing laparotomy or robotic surgical staging for endometrial cancer. Am J Obstet Gynecol 2016;214:350.e1-10.


20. Windberger U, Siegl H, Ferguson JG, Schima H, F├╝gger R, Herbst F, et al. Hemodynamic effects of prolonged abdominal insufflation for laparoscopic procedures. Gastrointest Endosc 1995;41:121-9.


21. Jakimowicz J, Stultiëns G, Smulders F. Laparoscopic insufflation of the abdomen reduces portal venous flow. Surg Endosc 1998;12:129-32.



22. Ball A, Bentley JR, OŌĆÖConnell C, Kieser KE. Choosing the right patient: planning for laparotomy or laparoscopy in the patient with endometrial cancer. J Obstet Gynaecol Can 2011;33:468-74.


23. Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med 2018;379:1895-904.


24. Bishop EA, Java JJ, Moore KN, Spirtos NM, Pearl ML, Zivanovic O, et al. Surgical outcomes among elderly women with endometrial cancer treated by laparoscopic hysterectomy: a NRG/Gynecologic Oncology Group study. Am J Obstet Gynecol 2018;218:109e1-11.

25. Krause AK, Muntz HG, McGonigle KF. Robotic-assisted gynecologic surgery and perioperative morbidity in elderly women. J Minim Invasive Gynecol 2016;23:949-53.


26. Madden N, Frey MK, Joo L, Lee J, Musselman K, Chern JY, et al. Safety of robotic-assisted gynecologic surgery and early hospital discharge in elderly patients. Am J Obstet Gynecol 2019;220:253.e1-7.


27. Oresanya LB, Lyons WL, Finlayson E. Preoperative assessment of the older patient: a narrative review. JAMA 2014;311:2110-20.


28. Delvecchio A, Conticchio M, Riccelli U, Ferraro V, Ratti F, Gelli M, et al. Laparoscopic versus open liver resection for hepatocellular carcinoma in elderly patients: a propensity score matching analysis. HPB (Oxford) 2022;24:933-41.


29. Manceau G, Brouquet A, Chaibi P, Passot G, Bouch├® O, Mathonnet M, et al. Multicenter phase III randomized trial comparing laparoscopy and laparotomy for colon cancer surgery in patients older than 75 years: the CELL study, a F├®d├®ration de Recherche en Chirurgie (FRENCH) trial. BMC Cancer 2019;19:1185.




-
METRICS

-
- 0 Crossref
- Scopus
- 716 View
- 74 Download
- Related articles in Obstet Gynecol Sci
-
Laparoscopic gynecological surgery in COVID-19 pandemic2021 May;64(3)
Minilaparotomy for gynecologic surgery.1991 September;34(9)
Clinical application of laparoscopy in gynecology.1993 July;36(7)
Seventy cases of endoscopic surgery in gynecologic patients.1993 November;36(11)
Diagnostic Laparoscopy in Infertile Patients.1997 October;40(10)




















