Factors related to dysmenorrhea among Vietnamese and Vietnamese marriage immigrant women in South Korea
Article information
Abstract
Objective
To find factors associated with dysmenorrhea, we surveyed the obstetric and gynecologic histories as well as socioeconomic factors of Vietnamese female residents in Can Tho (southern part of Vietnam) and Bavi (northern part of Vietnam) and Vietnamese female marriage immigrants living in South Korea.
Methods
From March 2010 to March 2011, 3,017 Vietnamese women aged 17 to 42 years (mean, 25.5 years) were recruited. Socioeconomic factors as well as baseline characteristics, including gynecologic history and menstrual patterns, were collected using questionnaires. The relationships between these factors and dysmenorrhea were analyzed using chi-square test, independent t-test and logistic regression analysis.
Results
Dysmenorrhea was found in 58.8% of all women. The mean age and the age at menarche were younger in the women with dysmenorrhea. A longer duration of menstrual flow and severe menstrual volume increased the risk of dysmenorrhea. The prevalence of dysmenorrhea was lower in women who had experienced pregnancy, term delivery and breastfeeding. The prevalence of dysmenorrhea in Vietnamese women was also different according to their educational status. When participants were divided according to their religious preferences, atheist women showed a lower prevalence with 55%, and women who were religious had a higher prevalence of dysmenorrhea. The body mass index, menstrual cycle length, monthly income, and duration of residency in Korea were not related with the prevalence of dysmenorrhea.
Conclusion
Socioeconomic factors as well as age, menstrual pattern and obstetric history were related with dysmenorrhea in Vietnamese women.
Introduction
Dysmenorrhea is characterized as a periodic menstrual cramping pain occurring in the center of the lower abdominal region. Dysmenorrhea is a common gynecological problem in women of childbearing age; in general, it begins with the first ovulation cycle, which occurs about two years after menarche. The prevalence is 60% to 90% in adolescent women, and it gradually decreases with age [1-6]. The condition can be classified into primary dysmenorrhea and secondary dysmenorrhea depending on the cause. Primary dysmenorrhea is due to the contraction of the myometrium without ovarian or cervical lesions; it appears either immediately before or after menstruation and continues for one to three days. This primary type is closely related to ovulatory menstruation; dysmenorrhea rarely occurs during the temporary anovulatory menstrual periods of menarche. Secondary dysmenorrhea is caused by a gynecological disorder and may also occur during anovulatory menstrual cycles. The known risk factors of primary dysmenorrhea are a body mass index (BMI) of 20 kg/m2 or less, early menarche before 12 years old, long menstrual intervals or long menstrual periods, massive menstrual volume, and smoking. Delivery experience is known to decrease dysmenorrhea, but having a miscarriage does not affect symptoms [6-12]. On the other hand, socioeconomic factors are associated with dysmenorrhea.
Recently, Korean society has resolved some socioeconomic problems, such as low fertility and late marriage, through international marriage and accepting immigrant workers. As a result, a rapid change to a multicultural society is occurring. International marriages between Korean men and Vietnamese women accounted for about 40% of the total international marriages; more than 13,000 Vietnamese women move to Korea to live. Because they are an important part of the Korean socioeconomy and they have significant roles in family composition, domestic Vietnamese marriage immigrants were investigated and compared to Vietnamese women living in the southern and northern regions; frequency of dysmenorrhea and factors affecting dysmenorrhea were evaluated, including socioeconomic factors.
Materials and methods
From March 2010 to March 2011, 3,017 Vietnamese women aged 17 to 42 years were investigated. The cohort was composed of 993 domestic marriage immigrants, 1,026 women living in the northern region of Vietnam (Bavi) and 998 women living in southern Vietnam (Can Tho). In the Korean provinces of Jinju, Okcheon, Gongju, Pohang, Gyeongju, Pusan, Masan, and Sangju, where many Vietnam marriage immigrants live, participants in this cohort study were recruited using advertising through the Marriage Immigrant Family Support Center and the Korean School for Marriage Immigrants. Information regarding the contents and items of examination as well as the procedure and introduction was mailed, then questionnaires were given and examinations were conducted on the day of examination. Participants received questionnaires written in Vietnamese, and an interpreter explained the contents if required before the women completed the questionnaires. Basic items such as age, height and weight, as well as the history of menstruation and pregnancy and delivery were investigated. In addition, life habits, such as drinking history, smoking history and exercise frequency, and socioeconomic factors, such as resident region, education, religion, and average gross income, were also assessed. This study was approved by the Institutional Review Board of Ewha University Mokdong Hospital. This study results were analyzed using the SPSS ver. 19.0 (IBM, Armonk, NY, USA), and continuous variables were expressed as mean ± standard deviation for the statistical analysis. Continuous variables for the target comparison were tested with independent t-test, while categorized variables used chi-square; each factor's dysmenorrheal risk factors were analyzed using logistic regression. When the P-value was less than 0.05 for all items, the result was considered to be statistically significant.
Results
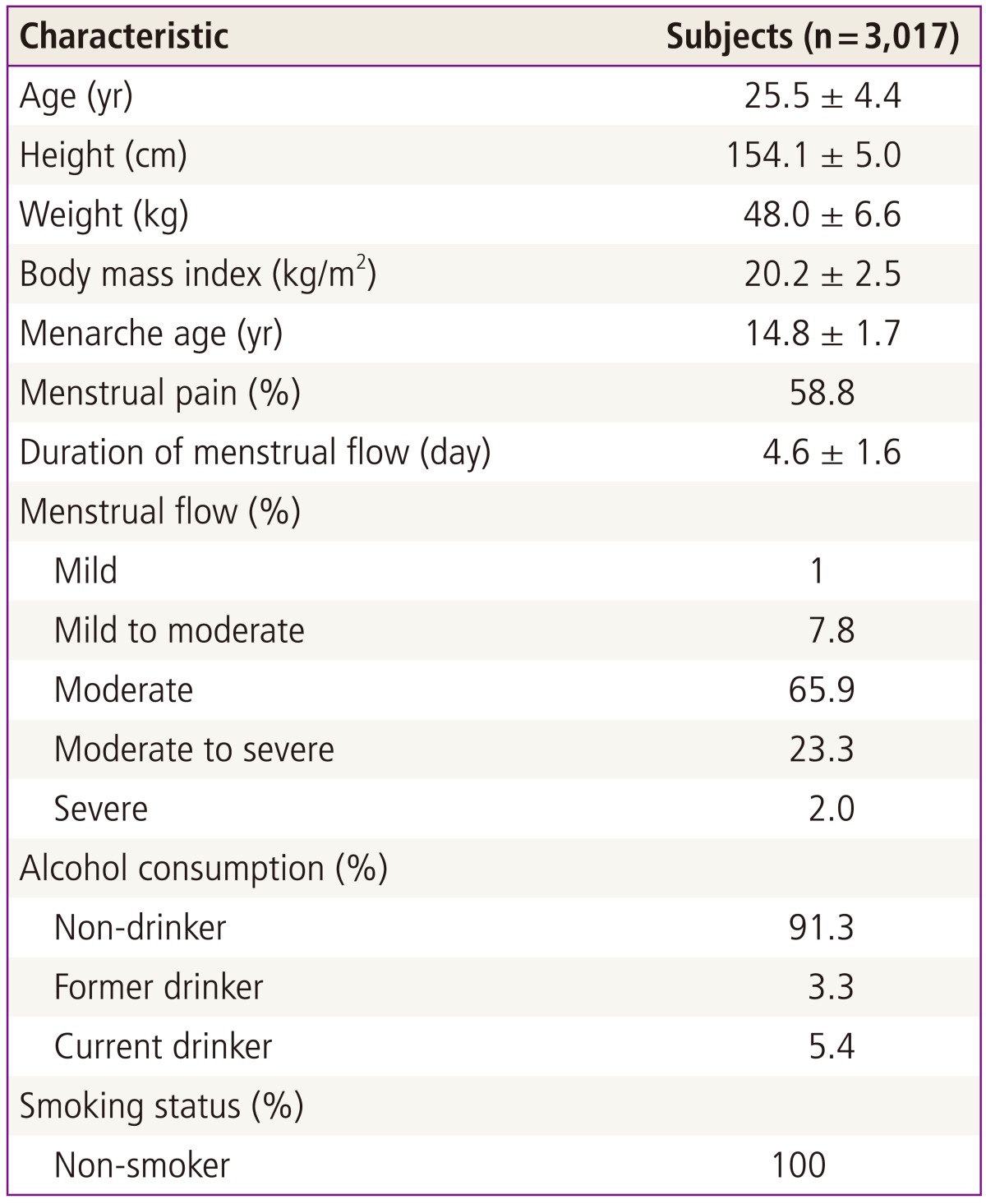
The average age of participants was 25.5 ± 4.4 years; the average age at menarche was 14.8 years. Women with dysmenorrhea made up 1,774 of the participants (58.8%), and the average BMI was 20.2 kg/m2. Most women (91.3%) did not drink alcohol, and all women who participated in the survey were non-smokers. The average menstrual period length was 4.6 ±1.6 days. The most frequently reported amount of menstrual volume was common (65.9%), followed by too much (23.3%) and a very large amount (2.0%) (Table 1).
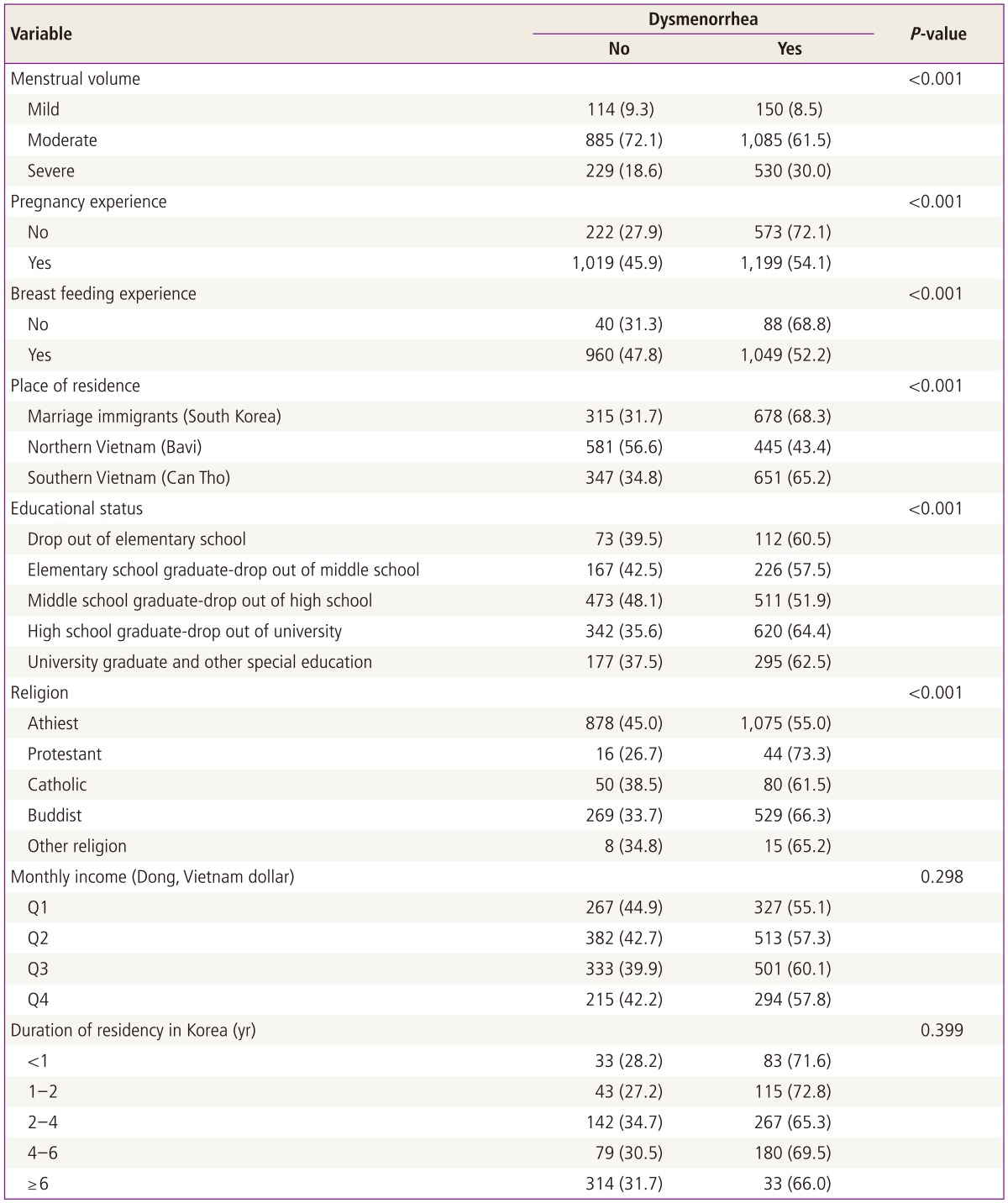
The average age of women without dysmenorrhea (24.9 ± 4.3 years) was significantly lower than the average age of women with dysmenorrhea (26.3 ± 4.4 years), and women without dysmenorrhea had a significantly lower age at menarche (14.7 ±1.8 years) than the age at menarche of women with dysmenorrhea (14.9 ±1.6 years); a younger overall age and a younger age at menarche were associated with higher amounts of dysmenorrhea. Women's menstrual intervals did not differ significantly according to the presence or absence of dysmenorrhea; women with dysmenorrhea had menstrual periods of 4.73 ±1.6 days, which was longer than those of women without dysmenorrhea (4.31±1.6 days). However, menstrual cycle and body mass index were not significantly associated with dysmenorrhea (Table 2). In women with highly massive menstrual volumes, the dysmenorrhea prevalence was significantly higher (30.0%) than in women without dysmenorrhea (18.6%) (Table 3).
Our investigation of the participants' delivery history and its association with dysmenorrhea revealed that experiencing pregnancy and breastfeeding produced a lower incidence of dysmenorrhea. We found that 72.1% of women without pregnancy experience showed dysmenorrhea, while only 54.1% of women who had been pregnant reported dysmenorrhea. The frequency of dysmenorrhea was also influenced by breastfeeding history; 52.2% of women who had breastfed a child showed dysmenorrhea compared to 68.8% of those who had not (Table 3).
The incidence of dysmenorrhea in northern Vietnamese residents at 43.4% was significantly lower than that reported by domestic marriage immigrants (68.3%) and residents of southern Vietnam (65.2%, P<0.001). When considering education, the high school graduation group had the highest frequency of dysmenorrhea (64.4%). A significantly low incidence was reported in the middle school graduation or high school dropout group (51.9%). The presence or absence of religion and religion-specific incidence of dysmenorrhea was also reviewed; women who were religious showed a higher incidence of dysmenorrhea than women who practiced no religion (55.0%, P<0.001); there was no difference among the type of religion practiced (Table 3). In contrast, the average monthly gross income and living period in Korea had no significant associations with dysmenorrhea.
Age, menstrual volume, pregnancy experience, resident region, education, and age at menarche were used for logistic regression analysis; the result was that dysmenorrhea was 1.847 times higher in women with massive menstrual volumes, and there was a significant correlation between massive menstrual volume and dysmenorrhea. Pregnancy lowered the risk of dysmenorrhea by about half (odds ratio [OR], 0.550; 95% CI, 1.349-2.501). Korean residents had a higher risk of dysmenorrhea than Vietnam residents overall, while southern Vietnam residents (OR, 0.590; 95% CI, 0.459-0.758) reported more dysmenorrhea than northern Vietnam residents (OR, 0.411; 95% CI, 0.338-0.499) (Table 4).
Discussion
This study was to conducted investigate the incidence of dysmenorrhea and socioeconomic factors affecting the dysmenorrhea occurrence in Vietnam women of childbearing age. Various factors were found to be significantly related with the incidence of dysmenorrhea. Age, age at menarche, menstrual period, and menstrual volume were correlated with dysmenorrhea, and a history of obstetric factors, such as pregnancy experience, full-term delivery and breastfeeding, as well as socioeconomic factors including resident region, education and religion, were significantly correlated with dysmenorrhea. BMI, menstrual period, average monthly gross income, and residence period in Korea did not show a clear association.
Various studies have investigated the current prevalence of dysmenorrhea. In a study of adolescents between 13 and 18 years, Wong discovered that one out of six experienced dysmenorrhea [13]. Banikarim et al. [14] reported an 85% prevalence of dysmenorrhea in Latin American women, and Sundell et al. [7] found an incidence of 72% in 19-year-old and 67% in 24-year-old Swedish women. Jamieson and Steege [15] reported 90% in 18-year-old to 45-year-old American women, and Lu [16] reported 51.3% in 15-year-old to 54-year-old Taiwan women [8]. This study was the first to determine the prevalence of dysmenorrhea in domestic Vietnamese marriage immigrants and Vietnamese resident women; the dysmenorrhea prevalence of Vietnamese women was similar (58.8%) with Turkish women of the same age (55.5% to 58.2%) [12,17].
In 1988, the dysmenorrhea prevalence amongst Korean high school girls was 77.8%, and it had fallen to 73.9% in 1998 [18]. This incidence was still higher than this study's finding of 58.8%, which might have been caused by the age difference. This study's participants had an average age of 25.5 ± 4.4 years. When we reanalyzed our data to include only 17-year-old and 18-year-old women in this study, the prevalence of dysmenorrhea was 78.3%, which confirmed that there was no difference between same-aged Korean high school girls and this study's result (data not shown).
The average age of women who experienced dysmenorrhea was lower compared to women without dysmenorrhea. When logistic regression analysis was done, the result was consistent that the risk of dysmenorrhea was 0.97 times lower as age increased (P<0.006). Therefore, it may be worthwhile to review the relationship between age at menarche and dysmenorrhea. In this study, the average age at menarche of the group who experienced dysmenorrhea was 14.7 ± 1.8 years old, which was significantly lower than the group who had no dysmenorrhea (14.9 ± 1.6 years old) (P=0.001). It might be inferred that early menarche produces more prevalent dysmenorrhea, which matches with the study of Andersch and Milsom [8] with Swedish women and Tangchai et al. [19] study with Thai adolescents. Another study reported that delayed menarche showed a high dysmenorrhea occurrence [20]. The association with early age at menarche and dysmenorrhea was thought to result from the fact that women who matured earlier showed similar hormone patterns with adults, and slower-maturing women had only a half ovulation efficiency.
The menstrual period was significantly longer in the dysmenorrhea group (P<0.05), but the correlation of menstrual cycle length and dysmenorrhea was not significant. This finding agrees with the study that showed no correlation between menstrual period regularity and dysmenorrhea [21], but it did not match up with the study that found women with irregular menstrual cycles, massive menstrual volumes and long menstrual cycles showed high incidences of dysmenorrhea [22]. The result was consistent with an existing report that revealed high menstrual volumes were significantly correlated with dysmenorrhea [8].
The correlation between weight and dysmenorrhea was somewhat contradictory; women who were underweight showed a high incidence of dysmenorrhea in our study, and another study found that dysmenorrhea of sub-standard weight women was 1.5 times higher than overweight or obese women [19,23]. However, a different study reported higher complaints of dysmenorrhea in obese participants [8]. BMI and dysmenorrhea had no significant correlation in this study, which was consistent with local study results among adolescents [21].
Pregnancy and breastfeeding experience was associated with a low frequency of dysmenorrhea. Our findings matched with other reports that showed a significantly lower incidence of dysmenorrhea in women who had a delivery history [7,8]. Our results also disagreed with another report that found miscarriages did not decrease the frequency of dysmenorrhea [8]. No report has investigated the correlation between breastfeeding and dysmenorrhea. Therefore, to uncover the existence of an association among obstetrics history, menstrual history and dysmenorrhea frequency, further research is required for miscarriage experience, delivery method, breastfeeding period, etc.
Socioeconomic factors, resident region and dysmenorrhea frequency were associated, but there was no correlation with the average monthly gross income. Place of residence also affected the frequency of dysmenorrhea; 68.3% of domestic marriage immigrants reported dysmenorrhea, while 65.2% of southern Vietnam residents and 43.3% of northern Vietnamese residents complained of the same symptoms. Similarly, our regression analysis result showed a lower risk of dysmenorrhea in northern and southern residents (0.411 and 0.459, respectively) compared to the Vietnamese domestic marriage immigrants; Vietnamese northern residents were at the lowest risk. The average monthly gross income was highest in Korea, and residents of the southern Vietnam region earned more income than those in the northern region. Therefore, these results could imply that socioeconomic status in each residence as well as resident region were correlated. However, the incidence of dysmenorrhea was not correlated with average monthly gross income (P=0.298), which agreed with the existing report [6] that showed no correlation between the incidence of dysmenorrhea and income but disagreed with the report [18] that indicated women with higher monthly gross incomes had a higher dysmenorrhea incidence than those making a lower monthly gross income. The association between dysmenorrhea and economic factors will need further research.
The limitations of this study were that we did not distinguish between primary dysmenorrhea and secondary dysmenorrhea, and mental types of socioeconomic factors, such as depression, stress, social isolation, etc., were also not considered. In addition, as the problem of co-linearity among various socioeconomic factors could not be ruled out, independent factors affecting the incidence of dysmenorrhea should be revealed through further analysis. Since the participants filled out the questionnaires independently, the possibility of recall bias and difficulty making an objective dysmenorrhea assessment cannot be ruled out completely. In further research on dysmenorrhea in different races, the dysmenorrhea prevalence could be surveyed with Korean women living in the same area compared to this study's Vietnamese marriage immigrant women.
In conclusion, this study showed that the incidence of dysmenorrhea was significantly correlated with age, menstrual history and obstetric history as well as socioeconomic factors, such as resident region, education and religion.
Notes
No potential conflict of interest relevant to this article was reported.