Comparison of midurethral sling outcomes with and without concomitant prolapse repair
Article information
Abstract
Objective
We compared the outcomes of the midurethral sling (MUS) with and without concomitant prolapse repair.
Methods
We retrospectively reviewed the outcomes of 203 women who underwent MUS at Severance Hospital from January 2009 to April 2012 with and without concomitant prolapse repair. Patients completed the urogenital distress inventory questionnaire preoperatively and postoperatively. The outcomes were assessed by using validated questionnaires and reviewing medical records. McNemar's test, t-test, and multiple logistic regression were used for analysis.
Results
We noted that women who underwent MUS alone were more likely to experience urinary frequency (12% vs. 25%, P = 0.045), urgency (6% vs. 24%, P < 0.001), and bladder emptying difficulty (2% vs. 10%, P = 0.029) compared to those who underwent concomitant repair. Women who only MUS were more likely to experience discomfort in the lower abdominal or genital region compared to those who than those who underwent concomitant repair; however, the difference was not significant (5% vs. 11%, P = 0.181). In the MUS only group, maximal cystometric capacity (MCC) was a significant parameter of preoperative and postoperative urinary frequency (P = 0.042; odds ratio, 0.994; P = 0.020; odds ratio, 0.993), whereas the Valsalva leak point pressure (VLPP) was a significant factor of postoperative bladder emptying difficulty (P = 0.047; odds ratio, 0.970).
Conclusion
The outcomes did not differ between patients who underwent MUS alone and those with concomitant repair. In the MUS only group, MCC and VLPP were significant urodynamics study parameters related to urinary outcome.
Introduction
Urinary incontinence (UI) is a common problem affecting between 12.8% and 46.0% of adult women [1]. Stress urinary incontinence (SUI), frequently occurs among healthy women-approximately 30% of these women are aged <30 years and 14% to 41% of these women are aged 30 to 60 years. The prevalence of UI increases with age, ranging from 12.2% in women aged 60 to 64 years to 20.9% in those aged >85 years [2]. The midurethral sling (MUS) is the treatment of choice for SUI as it is minimally invasive, associated with a shorter recovery times, and results in fewer perioperative complications [3,4]. Moreover, pelvic organ prolapse (POP) is often a comorbid condition in women with UI and reportly occurs in 15% to 80% of UI patients [5].
Thus, several studies have been conducted to determine whether concomitant POP repair is effective for patients with SUI. Researchers have hypothesized that damage to similar anatomical structures leads to the loss of both pelvic support and continence; however, this hypothesis does not explain the underlying cause among those women who experience prolapse or incontinence alone. In a study conducted by Richter et al. [6], women with preexisting SUI at the time of prolapse repair had significantly lower urinary tract symptoms, suggesting that concomitant SUI and prolapse represent a marker for more severe pelvic floor disorders.
However, some studies have described the outcomes of MUS and concomitant prolapse repair in patients with SUI and have indicated that efficacy and improvement in quality of life in these patients is similar to that in patients treated with MUS alone [7-9]. However, the data on patients with mixed UI who are treated with MUS and concomitant POP repair are scarce. Thus, the efficacy of concomitant surgery remains controversial.
In the present study, we compared the urinary outcomes between patients with UI who underwent MUS alone and those with POP who underwent MUS with concomitant prolapse repair. Moreover, we also examined the effect of concomitant surgery on postoperative urinary outcomes. In addition, we performed urodynamic studies (UDS) preoperatively, and the relationship between UDS parameters and postoperative urinary outcomes was assessed.
Materials and methods
In this retrospective cohort study, we included 212 patients who underwent MUS, involving the use of a transobturator tape, with and without concomitant prolapsed repair from January 2009 to April 2012 at Yonsei University Severance Hospital. Among these patients, 9 patients were excluded for the following reasons: did not undergo UDS preoperatively, lack of urogenital distress (UDI-6) data, or loss to follow-up. Eventually, the medical records of 203 patients were reviewed.
The UI in patients was preoperatively confirmed by physical examination, and also on the findings of UDS in cases where it was indicated. Physical examination included prolapse, atrophy, levator muscle palpation (symmetry and ability to squeeze), anal sphincter function, and the Q-tip test.
All the patients underwent surgery via the vaginal approach. However, patients who underwent MUS with POP repair were excluded. The objective outcomes were assessed by UDS findings, blood loss, duration of hospital stay, operative time, and pre/post POP-Q staging. The subjective outcomes were assessed using the UDI-6 questionnaire. The short form of the UDI-6 was completed during the preoperative and postoperative assessments. Patient demographics were recorded for the assessment of preoperative, intra-operative, and postoperative parameters. The UDI-6 is a validated condition-specific questionnaire that has been used in patients undergoing pelvic reconstructive surgery to compare the preoperative and postoperative patient status. The questionnaire contains 6 questions that assess the degree to which a patient is affected by symptoms such as UI (question 1), SUI (question 2), urge incontinence (question 3), small amounts of urinary leaking (question 4), difficulty in bladder emptying (question 5), and pelvic pain/discomfort (question 6). Patients completed the UDI-6 at 4 months postoperatively. Pelvic examination was performed at 1, 4, and 6 months postoperatively. The patients were also assessed for POP-Q staging, dehiscence, and operative site bleeding.
All 203 patients underwent UDS preoperatively, and six parameters were compared to determine a significant difference in the outcomes between patients undergoing MUS with and without concomitant prolapse repair. These parameters included the Valsalva leak point pressure (VLPP), maximal urethral closing pressure (MUCP), maximal flow rates (Qmax), detrusor pressure at maximal flow (PdetMax), maximal cystometric capacity (MCC), and postvoidal residual volume (PVR).
Data were analyzed using McNemar's test and the two-sample t-test. Patient demographics and clinical characteristics were controlled. If the P-value was <0.1 on univariate analysis, multivariate logistic regression was performed to determine the effect of concomitant POP on the outcomes of MUS. Institutional review board approval was obtained for this study.
Results
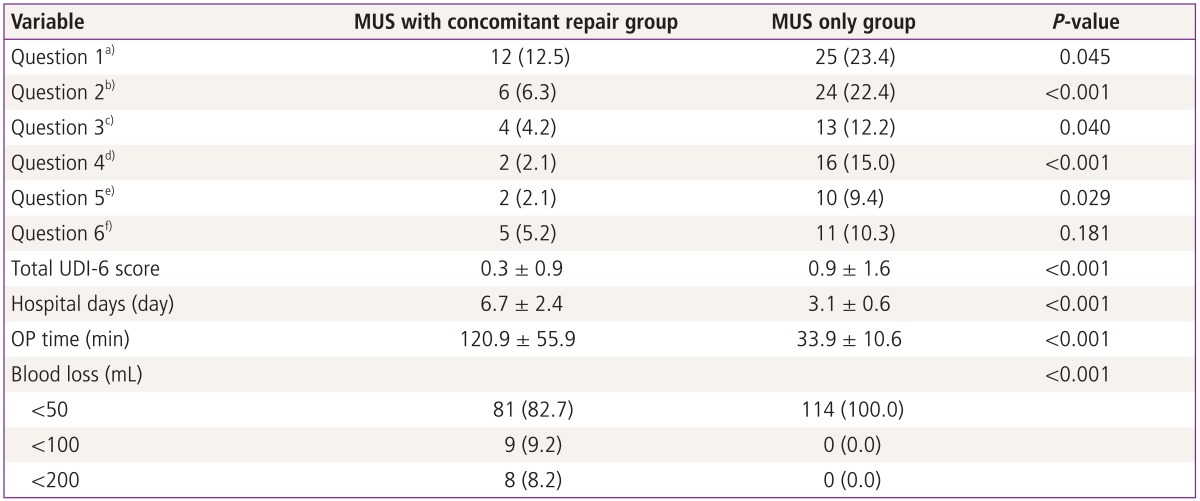
In total, 203 of the 212 (95%) women who underwent MUS between January 2009 and April 2012 completed the follow-up survey and were included in the study. Of these women, 114 (56%) underwent MUS only and 98 (48%) underwent MUS with concomitant pelvic floor repair. The women in the concomitant repair group were significantly older than those in the MUS only group (median age, 61 vs. 54 years, respectively; P < 0.001). Moreover, the women in the concomitant repair group showed increased parity (4.5 vs. 3.8, P = 0.017), diabetes mellitus (11.2 vs. 3.5, P = 0.029), hypertension (48.0 vs. 23.7, P < 0.001), mixed UI (20 vs. 5, P < 0.001), requirement of anti-cholinergic medication (21 vs. 9, P = 0.009), and incidence of having home delivery or difficult labor (39 vs. 19, P < 0.001) as compared to those in the MUS procedure only group, respectively. The groups did not significantly differ in terms of body mass index, body weight or prior pelvic surgery (Table 1). In the concomitant repair group, the most common type of POP-Q staging was IIIBa (39 women, 41%). The second-most common type of POP-Q staging was IVC (18 women, 14%) (Fig. 1). In addition, the women underwent concomitant repair had a significantly longer duration of hospital stay (6.7 ± 2.4 vs. 3.1 ± 0.6, P < 0.001), and increased blood loss (<50 mL; 81 vs. 114, P < 0.001), and operative time (120.9 ± 55.9 vs. 33.9 ± 10.5, P < 0.001) compared to the MUS only group, respectively.

Differences in the characteristics between the mid-urethral sling (MUS) only group and the MUS with concomitant repair group
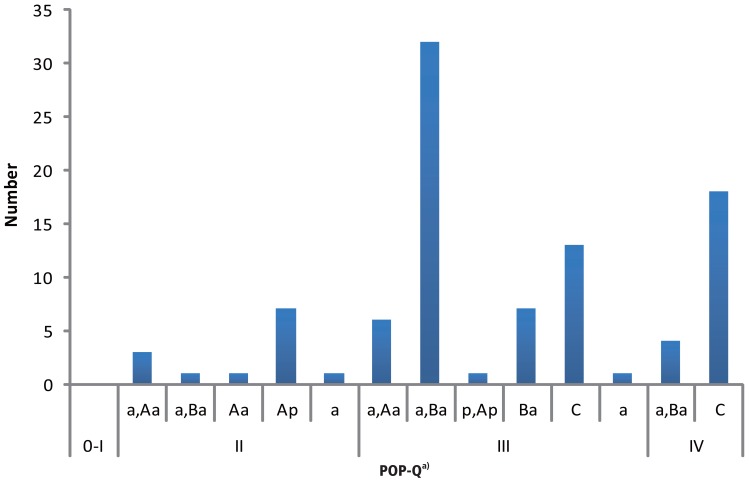
Preoperative pelvic organ prolapsed (POP)-Q staging of the midurethral sling with concomitant repair group. a)POP-Q stage. 0: No prolapse is demonstrated. Points Aa, Ap, Ba, and Bp are all at -3 cm, and point C is between the total vaginal length (TVL) and TVL -2 cm. I: The most distal portion of the prolapse is >1 cm above the level of the hymen. II: The most distal portion of the prolapse is <1 cm proximal or distal to the plane of the hymen. III: The most distal portion of the prolapse is <1 cm below the plane of the hymen but no further than 2 cm less than the TVL. IV: Complete to nearly complete eversion of the vagina. The most distal portion of the prolapsed protrudes to more than (TVL-2) cm. Aa: Anterior wall 3 cm from the hymen, -3 cm to +3 cm. Ba: Most part of the rest of the anterior wall, -3 cm to +TVL. C: Cervix or vaginal cuff ±TVL. D: Posterior fornix (if no prior total hysterectomy) ±TVL. Ap: Posterior wall 3cm from the hymen, -3 cm to +3 cm. Bp: Most part of the rest of the posterior wall, -3 cm to +TVL.
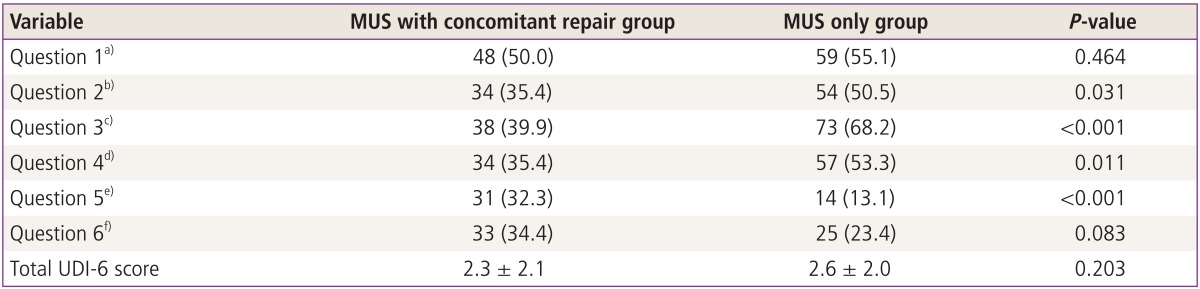
The MUS only group had a higher mean total UDI-6 scores as compared to the concomitant repair group, although this difference was not statistically significant (2.6 ± 2.0 vs. 2.3 ± 2.1, respectively; P = 0.203).
The postoperative total UDI-6 scores were significantly higher in the MUS only group than in the concomitant repair group (0.9 ± 1.6 vs. 0.3 ± 0.9, respectively; P < 0.001). Women who underwent MUS only tended to be affected by urinary urgency to a greater extent preoperatively and postoperatively (54% vs. 34%, respectively; P = 0.031; 24% vs. 6%, respectively; P < 0.001) and were more likely to experience in difficulty emptying the bladder postoperatively (10% vs. 2%, P = 0.029) compared to those who underwent concomitant repair, respectively.
In addition, the patients who underwent MUS only indicated a significantly greater difficulty in bladder emptying than those who underwent concomitant repair (2% vs. 10%, respectively; P = 0.029). Women who underwent MUS only were more likely to experience discomfort in the lower abdominal or genital region as compared to those who underwent concomitant repair, although this difference was not significant (5% vs. 11%, respectively; P = 0.181) (Tables 2, 3). On postoperative pelvic examination, only 1patient showed recurrence (preoperative POP-Q staging, IVC; postoperative POP-Q staging, IIAp).
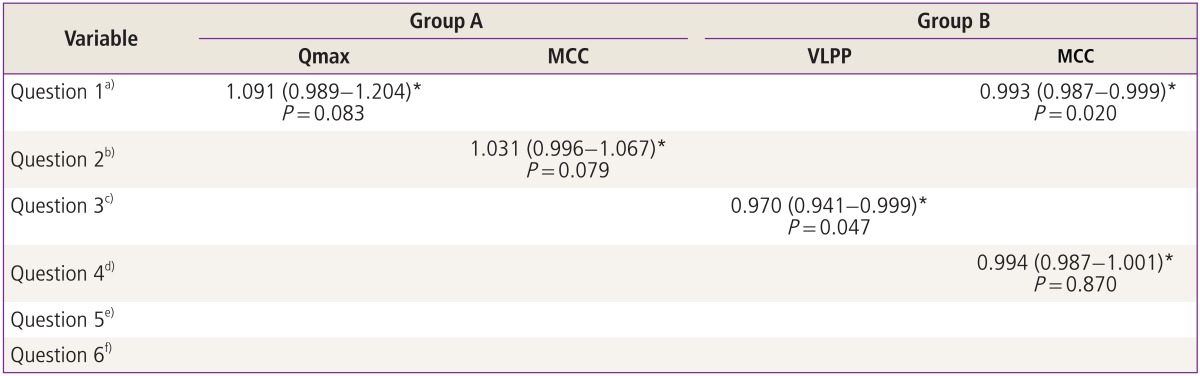
We compared 6 preoperative UDS parameters (VLPP, MUCP, Qmax, PdetMax, MCC, and PVR) to determine the significant differences in the outcomes between the 2 groups. MCC was found to be a significant parameter for urinary frequency, both preoperatively and postoperatively (P = 0.042; odds ratio, 0.994; P = 0.020; odds ratio, 0.993). Moreover, VLPP was found to be a significant factor for postoperative difficulty in bladder emptying (P = 0.047; odds ratio, 0.970). The differences in the other parameters between the 2 groups were not significant (Tables 4, 5).
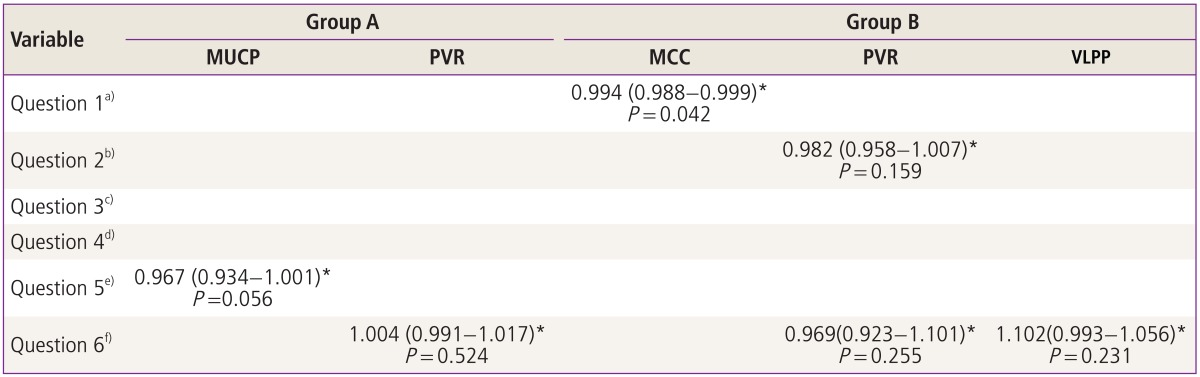
Correlations between UDS parameters and preoperative UDI-6 scores in the MUS only group (group A) and the MUS with concomitant repair group (group B)
Discussion
UI has been reported to coexist with POP in 15% to 80% of cases [5]. The treatment of coexisting POP when performing the MUS procedure for SUI has been found to be effective, and yields a similar improvement in symptoms compared to cases undergoing MUS alone [7-11]. Sokol et al. [12] and Yip and Pang [13] did not identify any significant difference in SUI cure rates between women who underwent concomitant prolapse repair during transvaginal tape and those who did not. Our data indicated a similar outcome with regard to UI cure rates with MUS during POP repair. Women who underwent MUS only tended to be affected by urinary frequency to a greater extent (12% vs. 25%, P = 0.045) and were more likely to have urgency (6% vs. 24%, P < 0.001) as compared to those who also underwent concomitant POP repair, respectively.
Despite the high success rates achieved when concurrently treating UI and POP, Huang et al. [10] and Partoll [11] reported that concomitant surgery causes postoperative side effects such as voiding difficulty, bladder outlet obstruction, and overactive bladder. Interestingly, the present data indicated that patients who underwent MUS only, exhibited a significantly greater difficulty in bladder emptying than those who underwent concomitant POP repair (2% vs. 10%, respectively; P = 0.029). Moreover, women who underwent MUS only were more likely to experience discomfort in the lower abdominal or genital region than those who underwent concomitant repair, although this difference was not significant (5% vs. 11%, respectively; P = 0.181). Thus, our data indicate that the outcomes did not differ between the MUS only group and the MUS and concomitant repair group.
The effect of UDS findings on the choice, or outcome of surgery remains controversial. Several studies have assessed the efficacy of preoperative UDS parameters; in general, patients with higher preoperative MUCP values are known to have better surgical outcomes.
Moreover,the predictive value of VLPP is inconsistent. Kilicarslan et al. [14] noted that high VLPP scores were associated with better outcomes, whereas other studies have failed to prove any effect of preoperative leak point pressures on surgical outcomes [15,16]. Certain Korean doctors indicated that patients with preoperative Qmax <15 mL/sec have a tendency to experience postoperative voiding dysfunction [17]. However, other researchers have insisted that preoperative UDS parameters are not associated with postoperative urinary outcomes [18], whereas other studies have not shown any differences in surgical outcomes based on preoperative UDS parameters [19,20]. Despite the conflicting results of these studies, UDS is considered the most accurate method for predicting surgical outcomes. The data in the present study indicated that MCC was a statistically significant parameter of urinary frequency, both preoperatively and postoperatively (P = 0.042; odds ratio, 0.994; P = 0.020; odds ratio, 0.993). The VLPP was a statistically significant parameter of postoperative bladder emptying difficulty (P = 0.047; odds ratio, 0.970) in the MUS only group. Thus, these findings indicate that the preoperative UDS parameters of MCC, and VLPP could predict the outcomes of concomitant surgery.
The strengths of the present study included the larger sample size as compared to previous studies and the use of the short form of the UDI-6 for quantifying the subjective symptoms of patients. In addition, all surgeries were performed by the same surgeon at the same hospital, and we compared patients at similar POP-quantification stages. To our knowledge, the present study is the first to compare the outcomes of MUS with and without concomitant prolapse repair in Korean patients. However, 1 limitation of the present study should be carefully considered. The surgical outcomes could differ according to the type of anterior repair, posterior repair, or apical suspension; however, our study was insufficiently powered to assess these subgroups.
In conclusion, no differences were observed in the outcomes of patients in the MUS only group and those in the MUS with concomitant repair group. In the MUS only group, MSS and VLPP were the UDS parameters that were significant predictors of urinary outcome. Although the investigations on this topic are ongoing, the findings remain controversial. Therefore, additional studies on related aspects are required to evaluate the postoperative urinary outcomes. Moreover, a larger number of patients should be included in future long-term studies to objectively assess the effectiveness and outcomes of MUS with and without concomitant prolapse repair.
Notes
No potential conflict of interest relevant to this article was reported.