|
 |
- Search
| Obstet Gynecol Sci > Volume 57(3); 2014 > Article |
Abstract
A 39-year-old woman was referred to our hospital at 28+2 week gestation. Routine obstetric examination revealed a palpable pelvic mass. Initial investigation by magnetic resonance imaging demonstrated a huge solid mass with heterogeneous enhancement that completely filled the right side of the abdomen. She underwent two surgeries: a programmed cesarean section by Department of Obstetrics and Gynecology team and a laparotomy performed by the General Surgery team. Final diagnosis was de-differentiated liposarcoma (French Federation Nationale des Centres de Lutte Contre le Cancer grade 2/3). She has been treated with radiation therapy focusing on high risk area of retroperitoneum followed by adjuvant chemotherapy (doxorubicin and ifosfamide). Below is the full case with literature review.
Liposarcoma is one of the most common soft-tissue sarcomas occurring in adults between 40 and 70 years [1,2]. According to the World Health Organization (WHO), histological classification of liposarcoma is divided into five subtypes: well-differentiated, myxoid, round cell, pleomorphic, and de-differentiated [3].
Liposarcoma are usually found at the extremities, retroperitoneum, spermatic cord, testis, thorax, breast, mediastinum, omentum, mesentery, etc. [1]. Most patients are asymptomatic and sarcomas are usually found incidentally during abdominal exam. When symptoms are present, the palpable mass is most often painless [4]. Therefore, an early detection is often very challenging, especially for pregnant women who already have distended abdomen due to the pregnancy itself.
Complete surgical resection of the tumor is the best choice of treatment, but an individualized approach should be taken, according to gestational age, tumor location, fetus status and the patient's general condition. The effects of additional chemotherapy or radiotherapy after surgery are still controversial.
In this report, we present a case of a pregnant patient with a retroperitoneal liposarcoma that was treated by two different surgeries followed by chemo-radiotherapy.
A 39-year-old woman was referred to our hospital at 28+2 week gestation. During a routine obstetric examination, a palpable pelvic mass was detected. She has history of five miscarriages during 2005 to 2009. She was diagnosed with habitual abortion, but no significant abnormalities were identified for the cause of the recurrent miscarriages. The patient had menarche at the age of 14, after she had regular periods. Besides that, her past medical history was unremarkable; however, her grandfather died of stomach cancer, and her father died of melanoma.
The patient' body mass index (BMI) was 21.99 before pregnancy. When she presented to our hospital at 28+2 weeks pregnancy, her BMI was 30.09 with a good nutritional status. Ultrasonographies of the patient's utereus showed a live singleton fetus of 27 gestational weeks along with multiple uterine myomas. Both ovaries were grossly normal and in the retroperitoneal area, there were huge sized heterogeneous cystic solid masses.
The patient was then submitted to magnetic resonance imaging that demonstrated a large mass in the right retroperitoneal space. The abdominal-pelvic computed tomography (CT) revealed an approximately 27 cm sized solid mass that completely filled the right side of abdomen. Furthermore, it was compressing the right side kidney medially and looked as if it was extending to the anterior cortex of the kidney. However, there was no evidence of direct invasion to adjacent organ or metastasis (Fig. 1).
Laboratory findings showed mild leukocytosis and mild anemia. And other laboratory analysis revealed normal values of hepatic-renal function, urinalysis and electrolytes. Tumor marker studies showed increased alpha-fetoprotein of 204.3 ng/mL (normal range, 0 to 10), a normal CA-125 of 6.6 U/mL (normal range, 0 to 35), a normal carcinoembryonic antigen of 0.4 ng/mL (normal range, 0 to 7), and a normal CA-19-9 of 0.5 U/mL (normal range, 0 to 35).
At the time of diagnosis, the size of tumor was very large (35×26×17 cm) and it was rapidly enlarging with high chance of being malignant tumor. It was determined that an early removal of the tumor will enhance the safety of the patient as well as the fetus. After a thorough discussion with the General Surgery team for this case, it was decided to perform the cesarean section and tumor removal at two different stages to prevent excess blood loss, and for the complete tumor removal. Before the cesarean section, a betamethasone was given to promote fetal lung maturation. When the patient reached 29 weeks gestation, the patient underwent a programmed cesarean section and delivered a male baby weighing 1,180 g with Apgar scores of 4 and 6, at 1 and 5 minutes, respectively. During operation, left a paratubal cyst was incidentally founded and a left paratubal cystectomy was also performed. Her baby was admitted to the neonatal intensive care unit for proper management.
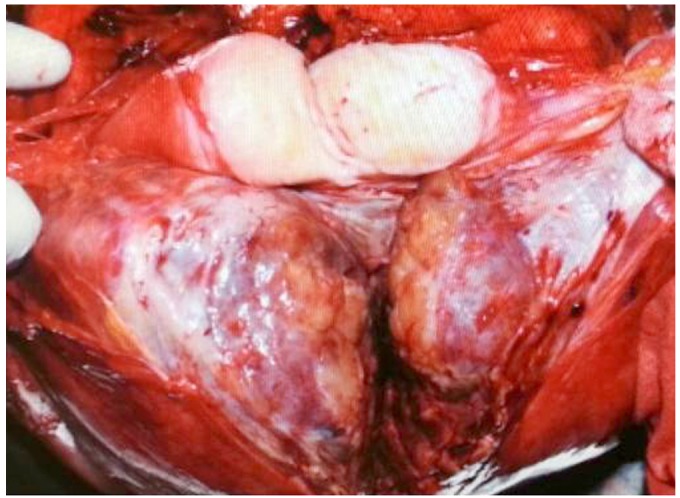
After, the patient was transferred to the General Surgery department for the proper treatment of her liposarcoma, and they performed another surgery at 22-days after cesarean section. The resected solid tumor was 35×26×17 cm in size with an intact capsule. However, there were necrotic tissues as well as dark-red colored hemorrhagic multiseptated cystic mass found inside the tumor. Frozen section showed a carcinoma with atypical cells. Thus mass excision, left nephrectomy, and appendectomy were performed. Final pathology revealed dedifferentiated liposarcoma (French Federation Nationale des Centres de Lutte Contre le Cancer grade 2/3) and the tumor was positive for MDM2, CDK4 and Ki-67 (Fig. 2).
The patient was discharged 15 days after surgical treatment without any immediate postoperative complications. Medical oncology was consulted, and additional radiotherapy and chemotherapy were recommended. Thirty days after the second surgery, she underwent thirty sessions of radiation therapy focusing on the high risk area of the retroperitoneum. Afterwards an additional chemotherapy with a regimen of doxorubicin Ifosfamide (doxorubicin 12.5 mg/m2, ifosfamide 2,000 mg/m2) was performed from December 2012 to February 2013. The last follow-up abdominal-pelvic CT was performed on February 28, 2013 which showed no evidence of disease. Thus, she has planned to follow-up after 3 month.
Liposarcoma is one of the most common soft-tissue sarcomas that frequently occur between the ages of 40 to 70 years [1,2]. Usually it is located at lower extremities and the retroperitoneum. This tumor's strongest prognostic factor is the pathologic grade of its histological subtypes, and its overall survival rate is reported as 23% to 46% [5].
Liposarcoma during pregnancy is extremely rare and often discovered incidentally by abdominal or pelvic ultrasound exam. The most common clinical feature is an asymptomatic palpable mass, which often is hidden and confused by the pregnancy itself [1]. The second most common symptom is pain, such as abdominal pain or pelvic pain [4]. The appropriate diagnostic and therapeutic approach to treat liposarcoma during pregnancy has not yet been determined; although, it is generally accepted that complete surgical resection of the tumor should be performed to increase the cure rate of this disease [6,7].
The prognostic factors are tumor size, location, surgical resection and histological subtypes. WHO classification divides liposarcomas into five subtypes: well-differentiated, myxoid, round cell, pleomorphic, and de-differentiated [3,8]. Well-differentiated is the most common subgroup that does not exhibit aggressive behavior and recur locally. Myxoid subtype is also a low-grade tumor with no aggressive behavior. Round cell subgroup are known to have intermediate behavior. While pleomorphic and de-differentiated tumors are known to be exceedingly aggressive with higher rates of metastasis and recurrence, and associated with poor prognosis [8].
In our case, the patient was performed cesarean section at 29 weeks gestation, followed by a complete surgical resection that included a left nephrectomy and appendectomy. The histological subtype of this tumor was consistent with dedifferentiated liposarcoma located in retroperitoneum with involvement of resection margin. The patient had no immediate postoperative complications and treated with additional chemotherapy at the medical oncology department.
As for the 29 week fetus, he was in the intensive care for 61 days and discharged without any serious complications. He plans to follow-up at Busan Paik Hospital.
Retroperitoneal liposarcomas are extremely rare in pregnancy with few cases reported [9,10]. Moreover, they are usually asymptomatic and often discovered only after they get larger in size [11]. Regarding the management of the liposarcomas during pregnancy, both mother and fetus need to be appropriately treated. Therefore, individualized approach based on the patient's trimester at the time of diagnosis, the histological type and grade of the tumor should be considered.
References
1. Enzinger FM, Weiss SW. Soft tissue tumors. 3rd ed. St Louis: Mosby; 1995.
2. Lopes RI, Machado M, Paz C, Santos AC, Rezende WW. Successful outcome of a surgically treated giant retroperitoneal liposarcoma during pregnancy. Arch Gynecol Obstet 2009;280:1067-1069. PMID: 19347344.


3. Fletcher CD, Unni KK, Mertens F. World Health Organization. International Agency for Research on Cancer. Pathology and genetics of tumours of soft tissue and bone. Lyon: IARC Press; 2002.
4. Boulay R, Podczaski E. Ovarian cancer complicating pregnancy. Obstet Gynecol Clin North Am 1998;25:385-399. PMID: 9629578.


5. Cody HS 3rd, Turnbull AD, Fortner JG, Hajdu SI. The continuing challenge of retroperitoneal sarcomas. Cancer 1981;47:2147-2152. PMID: 7226108.


6. Zagars GK, Goswitz MS, Pollack A. Liposarcoma: outcome and prognostic factors following conservation surgery and radiation therapy. Int J Radiat Oncol Biol Phys 1996;36:311-319. PMID: 8892453.


7. Matsuda S, Tanaka K, Harimaya K, Matsumoto Y, Sato H, Iwamoto Y. Treatment of myxoid liposarcoma in pregnancy. Clin Orthop Relat Res 2000;(376):195-199. PMID: 10906875.

8. Dalal KM, Kattan MW, Antonescu CR, Brennan MF, Singer S. Subtype specific prognostic nomogram for patients with primary liposarcoma of the retroperitoneum, extremity, or trunk. Ann Surg 2006;244:381-391. PMID: 16926564.



9. Tebes S, Cardosi R, Hoffman M. Liposarcoma complicating pregnancy. Gynecol Oncol 2001;83:610-612. PMID: 11733983.


10. Jeng CJ, Tzen CY, Huang WC, Yang YC, Shen J, Tzeng CR. Recurrent retroperitoneal myxoid liposarcoma during pregnancy: a case report and literature review. Int J Gynecol Cancer 2005;15:1235-1238. PMID: 16343222.


11. Lopes RI, Lopes RN, Barbosa Filho CM. Giant retroperitoneal liposarcoma. Braz J Urol 2002;28:227-229.
-
METRICS

-
- 13 Crossref
- 15,287 View
- 30 Download
- Related articles in Obstet Gynecol Sci
-
A clinical analysis of ectopic pregnancy.1991 February;34(2)
A case of fetus papyraceus in twin pregnancy.1991 February;34(2)
A case of mullerian adenosarcoma of endometrium.1991 February;34(2)
A case of huge endometrial cyst of the ovary.1991 February;34(2)