Can follicular fluid 8-oxo-2′-deoxyguanosine predict the clinical outcomes in ICSI cycle among couples with normospermia male?
Article information
Abstract
Objective
Oxidative stress (OS) occurs when excess free radicals damage the DNA. Moreover, 8-oxo-2′-deoxyguanosine (8-OHdG) is a well-known biomarker for OS linked to cellular damage and gene instability. However, its role in female subfertility has not been properly assessed. We aimed to examine the level of OS represented by 8-OHdG based on the cause of subfertility and to test its correlation with reproductive hormones, intracytoplasmic sperm injection (ICSI) parameters, and outcomes.
Methods
A cross-sectional study examined 108 subfertile couples with endometriosis, polycystic ovary syndrome (PCOS), tubal factors, and unexplained infertility undergoing ICSI treatment with two different stimulation programs. We included couples whose partners had normal sperm parameters. Levels of follicular fluid (FF) 8-OHdG were correlated with the causes of subfertility and fertilization rates and compared between pregnant and non-pregnant cases.
Results
Based on the causes of subfertility, FF 8-OHdG was the highest among endometriosis cases, followed by PCOS cases. Furthermore, FF 8-OHdG was higher in non-pregnant (2.37±0.75 ng/mL) vs. pregnant (1.58±0.39 ng/mL), P<0.001. A two-way analysis of variance showed that only subfertility affected ICSI outcomes, whereas the stimulation program did not. FF 8-OHdG correlated positively with female age and inversely with estradiol and good-quality embryos. The receiver operating characteristic estimated 8-OHdG cutoff value of 1.8 ng/mL predicted clinical pregnancies with 86.7% sensitivity and 74.4% specificity (P<0.001).
Conclusion
Higher FF 8-OHdG levels negatively impacted ICSI outcomes. FF 8-OHdG discriminated between cases of clinical pregnancy with good specificity and sensitivity. Because OS can be measured and treated, this opens up a therapeutic and prognostic avenue for improving ICSI outcomes.
Introduction
Remarkable progress in assisted reproductive techniques (ART) has improved opportunities for subfertile couples [1]. Intracytoplasmic sperm injection (ICSI) is a significant breakthrough for couples with severe male-factor infertility. However, the data demonstrated a consistent increase in ICSI compared with conventional in vitro fertilization (IVF) techniques. This trend was not confined to male factor infertility but also to unexplained infertility, a low number of retrieved oocytes, and older women, with no strong evidence of its superiority to standard IVF in cases of non-male-related infertility [2]. A possible cause for this increase may be the total fertilization failure encountered in conventional IVF. Nevertheless, the overall risk/benefit analysis supports conventional IVF for non-male infertility [1,2].
Oxidative stress (OS) is an imbalance between pro-oxidant molecules such as reactive oxygen and nitrogen species and antioxidant defenses. Overall survival (OS) is crucial in male and female subfertility [3].
Furthermore, 8-hydroxy-2-deoxyguanosine (8-OHdG) is a well-known biomarker for OS. It is produced in response to DNA-base modifications. OS is vital in promoting final oocyte maturation and orchestrating follicular rupture. However, the overproduction of reactive oxygen species (ROS) and/or the imbalance between OS and antioxidative mechanisms can contribute to diverse infertility disorders and human diseases such as metabolic diseases, male and female infertility, polycystic ovary syndrome (PCOS), abortion, and preeclampsia [4,5].
ROS are produced within the follicle as a by-product of oxygen metabolism during the ovulatory cycle; DNA is the most common target for ROS and has been linked to cellular damage and gene instability. Antioxidants act as scavengers of the harmful effects of ROS and play a critical role in oocyte maturation [6]. Previous studies have shown that women with high rates of defective oocytes have elevated follicular fluid (FF) 8-OHdG concentrations compared with those with low rates. Others have reported that patients with PCOS have reduced serum 8-OHdG levels compared with matched controls [7].
ROS induces female subfertility via different pathways. The direct pathway triggers DNA damage in the ova. Ovarian follicles with excess ROS that exceed the physiological antioxidant defense mechanism consequently suffer from direct DNA damage, thus impairing fertilization odds. Steroidogenesis (follicle-stimulating hormone and estradiol) is another pathway of female subfertility that results in decreased oocyte quality and overall IVF success [5–7]. ROS tend to deplete glutathione; the latter is needed for the decondensation of sperm chromatin to form male pronuclei after IVF, in addition to supporting the blastocyte stage. Consequently, their absence causes antral follicle apoptosis and poor-quality oocytes [8].
FF is an important component of the oocyte microenvironment. FF accumulates in all metabolic processes throughout oocyte development, which are needed for oocyte development, follicular maturity, and germ cell-somatic cell connection. Oocytes and follicular somatic cells collaborate in the ovaries to maintain correct glucose, amino acid, and lipid metabolism [4]. It is reasonable to believe that the FF biochemical milieu is critical in determining oocyte quality and fertilization potential to produce good embryos [4,9,10].
The role of 8-hydroxy-2-deoxyguanosine in male infertility has been addressed; however, its role in female infertility has not been well studied. Despite major leaps in assisted reproductive technology, we still face a major and profound problem factor attributed to the imbalance of OS and anti-oxidative defense mechanisms [11]. Therefore, it is necessary to identify the confounding factors related to OS in ICSI cycles. Because infertility has many causes, this study was designed to assess OS (measured by FF 8-OHdG) based on the causes of infertility as a primary aim. The secondary aim was to estimate FF 8-OHdG’s potential correlation with reproductive hormones, ICSI outcomes, and the cutoff value linked to clinical pregnancy among couples with normal sperm parameters.
Materials and methods
A cross-sectional study was conducted from July 2019 to June 2020, and 108 subfertile couples were referred for ICSI procedures at the IVF Infertility Center of the University Hospital. The Ethics Committee of Mustansiriyah University/Faculty of Medicine approved this study (IRB 167; April 23, 2019). The couples were briefed about the aims and procedures of the study. Informed consent was obtained from all patients, and the Declaration of Helsinki was followed.
1. Enrollment criteria
We included only couples with normal male partners; they were subsequently subdivided according to the subfertility causes (mild endometriosis, PCOS), tubal blockage, and unexplained infertility). Females ranged in age from 18 to 40 years, with body mass indexs (BMI) ranging from 18 to 30 kg/m2. All recruited couples had normal male seminal fluid based on World Health Organization (WHO) criteria for 2010 WHO criteria [12].
The patients’ histopathological and/or laparoscopy reports based on the American Society of Reproduction criteria confirmed the diagnosis of mild endometriosis. Women with endometriosis were subgrouped into stages II-IV. None of the female partners had endometriomas >3 cm in diameter. PCOS was confirmed using the Rotterdam criteria [13], and the tubal blockage was confirmed using hysterosalpingography and/or laparoscopy. Unexplained infertility was defined as the absence of male and female abnormalities, including normal ovulation, tubal patency, and seminal fluid analysis [14].
Exclusion criteria were as follows: 1) abnormal seminal fluid parameters; 2) abnormal uterine structure, congenital malformation, or documented pathology, such as fibroid or moderate-to-severe endometriosis; 3) associated medical comorbidities, including thyroid diseases, diabetes, chronic inflammation, and liver and kidney disease; 4) drug intake, such as steroids; and 5) female BMI >30 kg/m2.
The couples were briefed about the aims and procedures of the study. Informed consent was obtained from all patients, and the Declaration of Helsinki was followed. For male partners, the medical and surgical history was revised, and a sample of seminal fluid was sent for analysis. It was considered normal according to the WHO criteria 2010 [12]. For female partners, a detailed history and physical examination were undertaken, including height and weight, to calculate the BMI.
2. Controlled ovarian stimulation
Day 2 (D2) serum hormones of the menstrual cycle were estimated, including follicle-stimulating hormone, luteinizing hormone, and estradiol (follicular stimulation hormone [FSH], luteinizing hormone [LH], and estradiol [E2]).
Two protocols were used for ovarian stimulation. Female partners were assigned to either the antagonist or short agonist protocols based on the female’s age, BMI, and cause of infertility [13].
We used the flexible antagonist protocol, where recombinant FSH (Merck Serono, Modugno [BA], Italy) was introduced via the subcutaneous route (SC) from D2 or 3 of the menstrual cycle daily until the E2 level exceeded 500 pg/mL, and the dominant follicle size was 14–15 mm. Herein, cetrotide 0.25 (Merck Serono, Halle, Italy) was injected SC daily until 3 dominant follicles >17 mm were achieved, where human chorionic gonadotropin (HCG) was introduced. The agonist protocol began on D2 of the cycle with daily administered decapeptyl at a dose of 0.1 mg/SC and continued till the triggering day. On D3, recombinant FSH was started at a daily dose of 150 international unit (IU)/SC and stopped one day before the triggering day.
The ovulation was triggered by introducing SC pregnyl (10,000 IU) once the E2 levels exceeded 1,500 pg/mL alongside a minimum of 3 dominant follicles of ≥17 mm at least 36 hours before the ova pickup day.
The ova was picked using ultrasound guidance, and FF was retrieved 36 hours after the trigger. The oocytes were separated from the FF and prepared for ICSI. Only mature oocytes at metaphase two were used for ICSI. The FF was centrifuged, and the clear supernatant was stored at −80°C to assess 8-OHdG as an OS biomarker. A, competitive-enzyme-linked immunosorbent assay Principle/Elabscience kit (Immuno-tech-Beckman Coulter, Webster, TX, USA) was used, according to the manufacturer’s instructions.
The fertilization rate was assessed 16–18-hour following sperm injection; the existence of two pronuclei (2PN) and extrusion of the second polar body confirmed fertilization. Two or 3 days after injection, the number and quality of embryos were examined and categorized using Veeck [15] criteria. A good-quality embryo was classified as one that had achieved the 4-cell stage on D2 and the 7-cell stage on D3 and had fragments filling less than 20% of its volume.
Only three top-quality embryos were transferred to subfertile women. To confirm a positive pregnancy, serum-HCG levels were measured 14 days after embryo transfer. Clinical pregnancy was defined as the presence of an intrauterine sac with a viable fetal heart 28 days after embryo transfer. The implantation rate was calculated as the number of positive HCG per total number of transferred embryos per group [16].
The number of retrieved oocytes, germinal vesicles, metaphase one oocytes, metaphase two oocytes (M2), 2PN, the quality and number of transferred embryos, and fertilization, implantation, and clinical pregnancy rates were recorded for analysis.
3. Statistical analysis
Continuous data were presented as means and standard deviations, while categorical variables were presented as numbers and percentages. Data normality was evaluated using the Shapiro-Wilk test. Continuous data were compared using (one-way analysis of variance [ANOVA]). Categorical variables were compared using the chi-squared test.
One-way ANOVA was used to compare the outcome of the ICSI program based on subfertility causes, and the FF 8-OHdG level was correlated with continuous data obtained in this study using linear regression, with a calculation of the associated coefficient of correlation and P-values. A two-way ANOVA test was used to show the effect of infertility causes and the stimulation protocol on 8-OHdG levels, with a calculation of the associated P-values. Logistic regression was constructed for the cause of infertility and its correlation with the successful pregnancy rate by calculating the associated odds ratio (OR) and 95% confidence intervals (CI). A receiver operating characteristic (ROC) curve was constructed to predict the cutoff value of FF 8-OHdG associated with successful pregnancy and its associated sensitivity and specificity. P-values less than 0.05 were significant. MedCalc version 20 was used for data analysis.
The required sample was estimated based on the following formula: sample size=(Z1-α/2)2×SD2/d2. Z1-α/2 is a standard normal variate (1.96); standard deviation (SD)=variable obtained from earlier studies [17]; d is absolute error calculated by the authors; sample size=1.962×0.42/0.12=3.84×0.16/0.01; required sample is 61 patients.
Results
A cross-sectional study recruited 108 subfertile couples with normal male partners, grouped according to female subfertility cause into the endometriosis group 12/108 (11%), tubal factor 22/108 (20.3%), PCOS 26/108 (24.03%), and unexplained infertility 48/108 (44.4%).
Concerning female demographic criteria, the mean age was 30.48±4.83 years (range 19–40), and the mean BMI was 25.72±2.23 kg/m2. Primary infertility affected 36/108 (33.33%) of the cases versus 72/108 (66.66%) who had secondary infertility; two stimulation protocols were used; 42/108 (38.88%) cases received the agonist protocol versus 66/108 (61.11%) that received flexible antagonist protocol. A positive clinical pregnancy was reported in 28/108 (25.92%) cases.
None of the hormones tested on D2 (FSH, LH, or estradiol) were statistically significant in the subgroup analysis, as shown in Table 1.

The basal hormonal analysis of study participants on day 2, grouped according to subfertility causes
Regarding the ICSI parameters, only the number of retrieved oocytes and oocytes in metaphase II were statistically significant between each group, as confirmed by a post-hoc test, with P-values of 0.002 and 0.006, respectively, as described in Table 2.
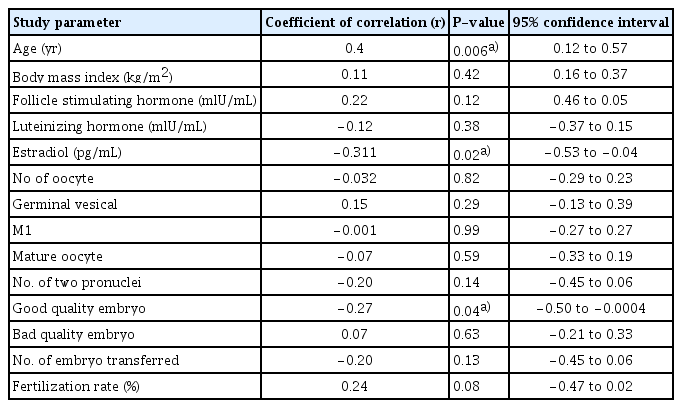
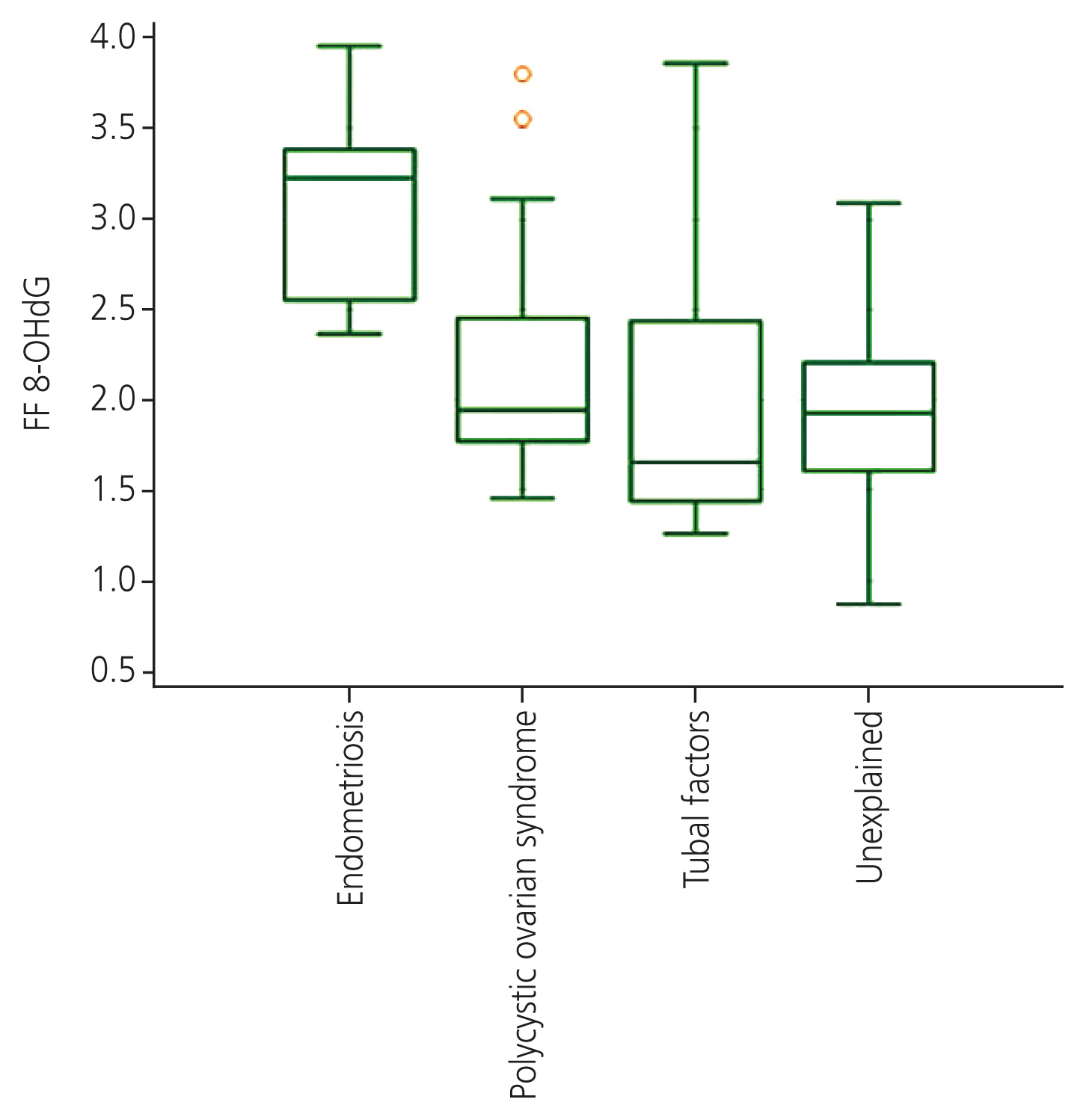
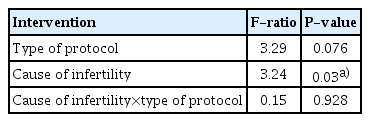
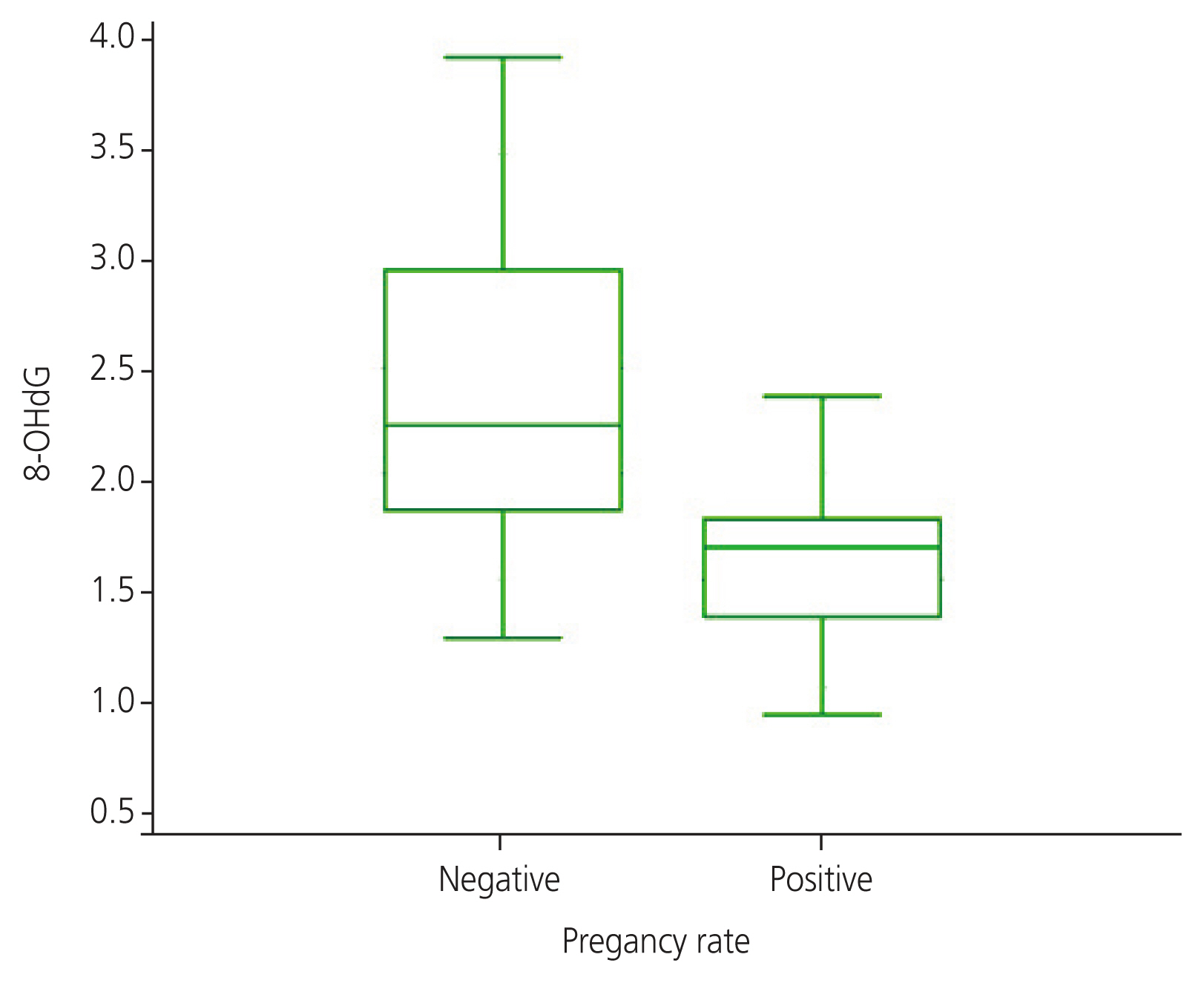
The FF 8-OHdG levels showed significant differences P<0.002 based on the cause of infertility. Endometriosis had the highest concentration, followed by PCOS and tubal factors, whereas unexplained infertility had the lowest FF 8-OHdG levels, as shown in Fig. 1. Using logistic regression, we calculated the OR for a positive pregnancy test, with the respective 95% CI and P-value described in Table 3. PCOS cases showed a trend of high OR for positive pregnancy (2.22; 95% CI, 0.19–25.72; P=0.52), followed by unexplained infertility, tubal factors, and endometriosis group; the latter was taken as the reference group. To test the influence of different stimulation programs and their interaction with the cause of infertility in the study participants, a two-way ANOVA was used; it confirmed that only the causes of infertility were significant (P=0.03), while the type of stimulation protocol failed to score statistical differences, as shown in Table 4. The level of FF 8-OHdG was significantly higher in non-pregnant (2.37±0.75 ng/mL) vs. pregnant (1.58±0.39 ng/mL), P<0.001, as shown in Fig. 2. Correlation analysis showed that FF 8-OHdG was significantly correlated with female age (0.4; P=0.006), D2 estradiol levels (−0.311; P=0.02), and good-quality embryos (−0.27; P=0.04) (Table 5). The ROC curve estimated an 8-OHdG cutoff value of 1.85 ng/mL linked with the highest sensitivity and specificity (86.7% and 74.4%; respectively), an area under the curve (AUC) of 0.83, and P=0.001 in predicting clinical pregnancy, as illustrated in Fig. 3.
The level of FF 8-OHdG based on the causes of subfertility. FF, follicular fluid; 8-OHdG, 8-oxo-2′-deoxyguanosine.

A multi-variant logistic regression and odds ratio for causes of infertility and their effect on pregnancy rate
A two-way ANOVA showing the effect of stimulation protocol and cause of infertility on ICSI outcome.
The level of FF 8-OHdG in non-pregnant vs. pregnant. 8-OHdG, 8-oxo-2′-deoxyguanosine; FF, follicular fluid.
Discussion
The analysis highlighted significant differences in the numbers (No.) of retrieved oocytes and M2 and FF 8-OHdG levels based on the cause of infertility. FF 8-OHdG had the highest concentration among the endometriosis groups, followed by the PCOS group. The OR for clinical pregnancy was the highest among PCOS cases and lowest in the endometriosis group. Only subfertility affected ICSI outcomes, whereas the stimulation program had no effect. FF 8-OHdG levels were significantly higher in non-pregnant women than in pregnant women. This confirmed strong positive correlations with female age and inverse correlations with E2 and good-quality embryos. Finally, the ROC estimated an 8-OHdG cutoff value <1.85 ng/mL that predicted clinical pregnancies with 86.7% sensitivity, 74.4% specificity, and P<0.001.
Nishihara et al. [18] addressed the correlation between FF OS markers (8-OHdG) and antioxidant status (total glutathione) with ICSI outcomes and embryo transfer rates. In accordance with our results, patients with endometriosis had the highest FF for 8-OHdG.
Another study investigated IVF outcomes in two subgroups: with and without endometriosis. They confirmed an inverse correlation of FF 8-OHdG with good-quality embryos; however, they found no difference in 8-OHdG levels either in the FF or in the serum of pregnant vs. non-pregnant women. Furthermore, only FF 8-OHdG levels were significantly higher in the endometriotic group, whereas serum levels showed a trend toward 8-OHdG elevation [19].
Several studies have reported that women with endometriosis have poorer outcomes. Affected women have different stem cell compositions and proliferation, hormone sensitivity, invasiveness, and immunological modulation [18].
Furthermore, the endometrium of affected patients resists selective progesterone activity, which regulates decidualization and modifies local inflammatory reactions throughout implantation. This explains the poor outcome among the endometriosis group, as shown by our results showing higher FF 8-OHdG levels and the lowest OR for clinical pregnancy [18,19].
The OR for clinical pregnancy was the highest for the PCOS subgroup. Sova et al. [20] reported that patients with PCOS had considerably lower serum 8-OHdG levels than age- and BMI-matched healthy controls. These levels were further reduced by metformin therapy. The authors assumed that 8-OHdG is not only a result of oxidative DNA damage but also possesses ROS-suppressing capabilities in many in vitro experiments, implying that it may play a role in preventing OS and fine-tuning the reactivity to OS [20].
Fabjan et al. [21] reported that the FF (8-OHdG) concentration was significantly lower in patients with PCOS. They suggested that it was a good predictor of oocyte fertilization and maturation. The authors explained that high ROS levels would stimulate more antioxidant enzymes, reducing oxidative stress. Consequently, this prevents the interaction between ROS and DNA and reduces 8-OHdG formation. Many researchers have confirmed that the levels of several antioxidant enzymes are significantly higher in women with PCOS [22].
Many female diseases, such as endometriosis, tubal blockage, and polycystic ovary syndrome, are associated with free radicals that can damage DNA. Excess ROS may harm the endometrium.
Previous studies suggested that biomarkers related to OS fall into the following categories: 8-OHdG is classified as a sensitive measure of DNA damage and OS, which underpins oocyte damage and negatively impacts oocyte quality, fertilization, embryo grading, and endometrial adequacy [19–21]. Different causes of infertility result in different OS levels, mirrored by the 8-OHdG levels [1,4,7]. The effect of OS markers on infertility is only a small fraction of the puzzle; FF-OHdG is not the only marker that indicates OS in infertile couples. Other markers of OS marker their role in OS damage leading to infertility requires further research. No single OS marker has been recommended, nor how anti-oxidants contribute to effective ICSI results has been elucidated [6,8,11].
Few studies have discussed the potential association between oxidative stress, type of stimulation program, and IVF outcomes. Our data showed that infertility causes affected ICSI outcomes, while the stimulation program failed to have a significant effect. Tulić et al. [23] investigated the differences in the serum levels of OS parameters before and after agonist and antagonist stimulation. Patients without OS exhibited better IVF outcomes after stimulation. However, in line with our results, the ovarian stimulation program was not linked to any change in OS parameters or ICSI outcomes; they showed an insignificant difference in the rates of biochemical pregnancies, abortions, and live births for both subgroups.
In contrast, Thaker et al. [24] showed that the long-agonist program had a higher No. of retrieved ova in comparison with the gonadotropin-releasing hormone antagonist program. However, the number of women with a positive outcome was conversely low in the long-agonist regimen. The authors attributed this to a higher no of retrieved follicles, which may have contributed to implantation failure. For antagonist and short agonist programs, pregnancy rates were matched [24,25].
The analysis confirmed a significantly high FF 8-OHdG level among non-pregnant women, in line with an earlier study that linked OS biomarkers to failed pregnancies [26].
Another study showed that high FF 8-OHdG levels in women with low fertilization rates were linked to poor-quality blastocytes. The authors recommended FF 8-OHdG and total glutathione as reliable biomarkers for successful fertilization in assisted reproduction [18]. Many studies have discussed the complex correlation between ROS and antioxidant status in the FF. ROS are unwanted byproducts of biological oxidation. Low levels of ROS may serve as a physiological signaling pathway in the embryo [27]. However, once this delicate balance in FF between OS and antioxidant defense mechanisms is disturbed by the overproduction of free radicals and/or underproduction of antioxidants, the increase in free radicals in FF consequently causes poor oocyte quality and low fertilization rates [28,29]. Nishihara et al. [18] reported contradictory results; they showed an insignificant correlation between OS and antioxidant levels in positive pregnancies. Our data highlighted the highest OS among the endometriosis groups represented by FF 8-OHdG levels, followed by the PCOS, tubal, and unexplained groups. However, tubal factors had the lowest OR for becoming pregnant [18].
No single OS biomarker has been recommended, nor has the mechanism by which antioxidants contribute to successful ICSI outcomes been elucidated; therefore, the authors recommended individual estimation of OS markers and antioxidants simultaneously in the FF [30].
Várnagy et al. [19] showed that FF 8-OHdG levels were negatively correlated with No. of a good-quality embryo in a patient undergoing a stimulation program; however, they found no correlation between FF 8-OHdG levels and mature oocyte No. Likewise, Seino et al. [31] declared that granulosa cells 8-OHdG negatively correlated with ova, embryo quality, and fertilization rates. Another study confirmed that the FF 8-OHdG levels were significantly higher in patients with high-grade oocyte degeneration [32].
The influence of maternal age on egg quality and fertilization is a well-known phenomenon in female fertility and was positively linked to the follicular oxidative state in the current study. Maternal age inversely affects the success of the ICSI cycle. Da Broi et al. [33] found that women older than 38 years experience a decrease in growing follicles, oocyte quality, and changes in the quality of the surrounding cells, underlining the importance of FF. Furthermore, female aging is associated with increased ROS production, decreased antioxidant production, and oocyte competency [19].
Advanced maternal age is linked to increased oocyte and embryo aneuploidies, and OS triggers aneuploidy in animal models. Our results indicated a strong positive correlation between FF 8-OHdG levels and maternal age. This ominous alliance increases chromosomal abnormalities in the offspring [8,32–35].
The inverse correlations of FF 8-OHdG with E2 and good-quality embryos were in agreement with earlier research; serum E2 levels were correlated with FF OS biomarkers that inversely affect ovarian responses [26].
It has been suggested that the immunomodulatory action of estrogen limits OS and simultaneously upregulates endogenous anti-oxidants [36]. Furthermore, immature ovarian follicles are E2 dependent. Women with reduced E2 levels experience embryonic arrest, which explains their inverse correlation with good-quality embryos [37].
The cutoff value of FF 8-OHdG (<1.85 ng/mL) predicted clinical pregnancy with a sensitivity and specificity of 86.7% and 74.4%, respectively (AUC, 0.83 and P=0.001), making it a valuable marker for clinical use. Many markers for OS in the FF have been extensively examined because of their close correlation with fertilization and pregnancy potential in IVF patients. In addition, 8-OHdG is regarded not only as a byproduct of oxidative DNA damage but also for its ROS-suppressing ability, which implies its potential applications in mitigating and tuning the OS response [20].
Although the OR for becoming pregnant was higher in PCOS cases and lowest in endometriosis cases, the difference was not statistically significant. Furthermore, the implantation and clinical pregnancy rates did not differ significantly between the groups. Therefore, one may assume that FF 8-OHdG correlates with clinical pregnancy rates rather than the causes of infertility, which is worthy of further research.
Study strengths: this study addressed the correlation between the causes of infertility and the effects of different stimulation protocols. Furthermore, we used FF 8-OHdG rather than serum, a more sensitive marker of reproductive potential [18].
What is unique about FF 8-OHdG, besides its correlation with infertility, is that earlier studies discussed an additional prognostic value; its levels were reduced following metformin therapy in PCOS cases, which opens therapeutic and prognostic avenues, especially in PCOS cases [20]. OS can be treated, and optimizing couples’ conditions before embarking on ICSI cycles can alleviate many financial, psychological, and health complications related to failed IVF trials [1].
The strong positive correlation between FF 8-OHdG and maternal age implies that reducing OS will improve the ICSI outcome and prevent increased chromosomal abnormalities in the fetus. Additionally, FF 8-OHdG has been validated as a quantitative marker of ROS DNA damage in male sperm [38].
Study limitations: smoking is a recognized confounder of 8-OHdG levels. However, the effects of passive smoking on female partners have not been addressed. A high level of 8-OHdG mirrors the underlying oxidative DNA damage and may signify a decline in the DNA repair rate [39,40]. Because only ICSI cycles were studied, this may represent a source of bias in the general effect of FF 8-OHdG on ART outcomes. In addition, the subgroup analysis included a small number of endometriosis cases, which may have impacted the results; therefore, the current results should be interpreted with caution.
Although many pieces of the puzzle on how to optimize ICSI outcomes are missing, it seems that the crosstalk between infertility causes and OS biomarkers plays a decisive role in improving the outcome. FF 8-OHdG, an OS marker, was the highest among the endometriosis cases and was inversely related to estradiol levels and the number of good-quality embryos. It distinguished women with clinical pregnancies with high sensitivity and specificity. Further studies are warranted to determine its prognostic and therapeutic applications in ICSI treatment.
Notes
Conflict of interest
The corresponding author states no conflict of interest on behalf of all authors.
Ethics approval
It was issued by the Ethical Committee of Mustansiriyah University/Medical College. Reference No. 167 on April 23, 2019.
Patient consent
All couples gave informed written and verbal consent.
Funding information
None.