Hyperthermic intraperitoneal chemotherapy as consolidation treatment of advanced stage ovarian cancer
Article information
Abstract
Objective
To investigate the therapeutic efficacy of hyperthermic intraperitoneal chemotherapy (HIPEC) as consolidation treatment after completing first-line treatment in patients with advanced ovarian cancer.
Methods
A retrospective chart review was conducted on patients treated at the Comprehensive Gynecologic Cancer Center between January 2014 and 2019. Based on the inclusion criteria, 24 eligible patients who received HIPEC (paclitaxel 175 mg/m2, for 90 minutes, at 42°C) (HIPEC group) as consolidation treatment after terminating the adjuvant chemotherapy were identified. Another 24 patients who met the inclusion criteria and did not receive HIPEC were matched, representing the non-HIPEC group. Disease-free survival (DFS) and overall survival (OS) were examined between the two groups.
Results
The median DFS was 28.7 and 24.2 months in the HIPEC and non-HIPEC groups, respectively (P=0.688). The 3-year DFS rates in the HIPEC and non-HPEC groups were 39.5% and 32.6%, respectively. However, the median OS was not determined. The 5-year OS rates in the HIPEC and non-HIPEC groups were 86.2% and 81.3%, respectively (P=0.850). One patient developed grade 3 neutropenia. Other patients experienced mild adverse events after HIPEC.
Conclusion
This study suggests that consolidation HIPEC could not support the survival benefit after completing the first-line treatment for patients with advanced ovarian cancer, although no severe specific safety issues were found. Therefore, randomized trials evaluating consolidation HIPEC for the management of ovarian cancer are warranted.
Introduction
Ovarian cancer is considered to have the highest mortality rate among all gynecological malignancies. Due to the absence of specific symptoms in the early stage and reliable screening tests, the majority of patients are diagnosed at advanced stages, where cancer spreads beyond the ovaries to the peritoneal seeding [1]. The current standard treatment for advanced ovarian cancer involves maximum effort to reduce the tumor burden through optimal cytoreductive surgery (CRS), followed by platinum-based systemic chemotherapy. If upfront CRS is not feasible, interval debulking surgery (IDS) can be performed after three cycles of neoadjuvant chemotherapy [2]. Despite these standard treatments, most patients experience relapse and eventually die [3]. The 5-year survival rate of women diagnosed with advanced ovarian cancer has changed slightly over the past few years but is still around 20-30%. Therefore, several innovative attempts have been made to enhance the efficacy of conventional treatments and improve survival outcomes.
Intraperitoneal (IP) chemotherapy is one of the attempted methods. Tumors in advanced ovarian cancer primarily spread to the peritoneal cavity, the main site of tumor recurrence. Therefore, local treatment strategies appear to be an ideal approach. Intravenous (IV) chemotherapy combined with IP chemotherapy significantly improved progressionfree survival (24 vs. 18 months; P=0.05; risk ratio [RR], 0.80) and overall survival (OS; 66 vs. 50 months; P=0.03; RR, 0.75) compared with those of conventional IV chemotherapy in patients with optimally debulked stage III ovarian cancer [4]. IP chemotherapy increases drug concentration within the abdominal cavity multiple folds, and significantly delayed drug clearance from the peritoneal cavity prolongs the duration of drug exposure. However, some factors, including catheter-related problems, toxicities, and postoperative adhesions that may hinder penetration, have been identified as potential barriers to applying this approach in routine clinical practice [4,5].
Hyperthermic IP chemotherapy (HIPEC) is a modified and attenuated IP chemotherapy method that delivers chemotherapy into the peritoneal cavity during surgery under hyperthermic conditions. Delivering IP chemotherapy at the end of surgery and subsequent extraction can circumvent most drawbacks of IP chemotherapy while maintaining its advantages. Hyperthermia ranging from 42°C to 45°C has a cytotoxic effect on tumor cells, enhances the penetration of the chemotherapy, and induces tumor cell death via multiple mechanisms. These include impairment of DNA repair, inhibition of angiogenesis, and induction of apoptosis [6-8].
In 2018, van Driel et al. [9] reported a randomized phase III trial to evaluate the efficacy of HIPEC during IDS after neoadjuvant chemotherapy in patients with stage III ovarian cancer. A significant advantage in recurrence-free survival (14.2 vs. 10.7 months, P=0.003) and OS (45.7 vs. 33.9 months, P=0.002) was observed in the IDS with HIPEC group as compared to those in the IDS-alone group, without higher incidence of adverse events. Despite these encouraging results, the effectiveness of HIPEC as consolidation therapy remains controversial. Therefore, this study aimed to investigate the therapeutic efficacy of HIPEC as consolidation treatment after completing first-line treatment for patients with advanced ovarian cancer.
Materials and methods
A retrospective chart review was conducted on patients treated at the Comprehensive Gynecologic Cancer Center, Bundang CHA Medical Center, between January 2014 and 2019. A total of 49 patients undergoing HIPEC met the following inclusion criteria and were selected as study candidates: (1) pathological confirmation of stage III or higher epithelial ovarian, fallopian tube, or peritoneal cancer based on the International Federation of Gynecology and Obstetrics (FIGO) classification 2014 and (2) partial or complete response after the optimal primary CRS and 6-9 cycles of standard platinum-based adjuvant chemotherapy. Among them, 24 patients who received HIPEC as the consolidation treatment were classified into the HIPEC group, and 25 were excluded for the following reasons: HIPEC performed with primary CRS (n=1), IDS (n=11), or secondary CRS (n=9), and pathologic confirmation of pseudomyxoma peritonei (n=4). Another 24 patients who met the criteria and did not undergo HIPEC were matched to the non-HIPEC group. This study was approved by the institutional review board (CHA IRB 2018-11-049).
HIPEC was performed within 3 weeks after completion of adjuvant chemotherapy, based on the eligibility criteria. The patient was placed in the supine position in the operating room and administered general anesthesia. A midline incision was made and the peritoneal cavity was comprehensively explored. If any suspicious lesions were detected, they were surgically removed, and delicate adhesiolysis was performed. After confirming the absence of tumor remnants and adhesion formation, HIPEC was initiated using the open coliseum method. The procedure was performed by three gynecologic oncologists (J. M. L, C. L, and M. C. C.).
Paclitaxel was administered intraperitoneally at a dose of 175 mg/m2 and mixed in 2,500-3,000 mL of normal saline. The diluted solution was heated at a target temperature of 41.5-42.0°C and continuously circulated into the abdominal cavity using a Belmont hyperthermic infusion pump (Belmont Instrument Corporation, Billerica, MA, USA). The temperature was measured using two IP probes. Two inflow tubes were placed in the pelvis and upper abdominal cavity at an infusion rate of 1,000 mL/min, whereas two other outflow tubes were placed in both paracolic gutters. The perfusion procedure was maintained for 60-90 minutes after 10 minutes of pre-heating. After completing the circulation procedure, chemotherapy-diluted fluid was extracted, and the cavity was irrigated with lactated Ringer’s solution. After thorough hemostasis and identification of the impaired site, the incision site was closed layer-by-layer.
Patients who were confirmed with any residual pathologic results from biopsy or peritoneal cytology received 3-4 cycles of additional chemotherapy after recovery from HIPEC. Disease-free survival (DFS) was defined as the time interval from the completion of first-line treatment to the clinical, radiological, or serological recurrence of progression, whereas overall survival (OS) was defined as the time interval from the completion of the first-line treatment to the occurrence of all-cause death in the HIPEC and non-HIPEC groups. Data were censored at the date of the last contact for patients who remained alive and had no evidence of disease progression. The cutoff date for the data was set on April 30, 2021.
All statistical analyses were performed using IBM SPSS ver. 20.0 for Windows (IBM Corp., Armonk, NY, USA). Patient demographics analysis was conducted using the chi-squared test and analysis of variance. DFS and OS analyses were performed using the Kaplan-Meier method. Statistical significance was set at P<0.05.
Results
1. Patient characteristics
The clinicopathological characteristics are presented in Table 1. No statistical differences were observed in the body mass index, peritoneal cancer index score at the initial surgery, FIGO stage, tumor grade, histology, germline BRCA mutation status, and further treatment with target agents between the two groups. The median age of the non-HIPEC group was 6.7 years older than that of the HIPEC group (55.9 years vs. 49.2 years, P=0.038). As a result of the germline BRCA test (specific test method was described in detail in a previous article [10]), mutations were found in approximately onethird of patients (29% and 38% in the HIPEC and non-HIPEC groups, respectively). No difference was observed in patients who received bevacizumab or olaparib (one of the approved poly ADP-ribose polypmerase inhibitors in Korea) after HIPEC between the two groups.
In the HIPEC group, ten patients had positive results for residual tumors from biopsy or peritoneal cytology during HIPEC. They received 3-4 cycles of maintenance platinum-based chemotherapy after recovery from HIPEC.
2. DFS and OS
A total of 13 (54.2%) and 15 (62.5%) patients in the HIPEC and non-HIPEC groups, respectively, had experienced recurrence during the median follow-up of 47.6 months, with a median DFS of 28.7 (95% confidence interval [CI], 14.1-43.2) and 24.2 (95% CI, 12.0-36.3) months, respectively (P=0.688) (Fig. 1A), but without significant differences. The 3-year DFS rates in the HIPEC and non-HPEC groups were 39.5% and 32.6%, respectively. Four (16.72%) and three patients (12.5%) died in the HIPEC and non-HIPEC groups, respectively. However, the median OS was not reached. The 5-year OS rates in the HIPEC and non-HIPEC groups were 86.2% and 81.3%, respectively (P=0.850) (Fig. 1B).
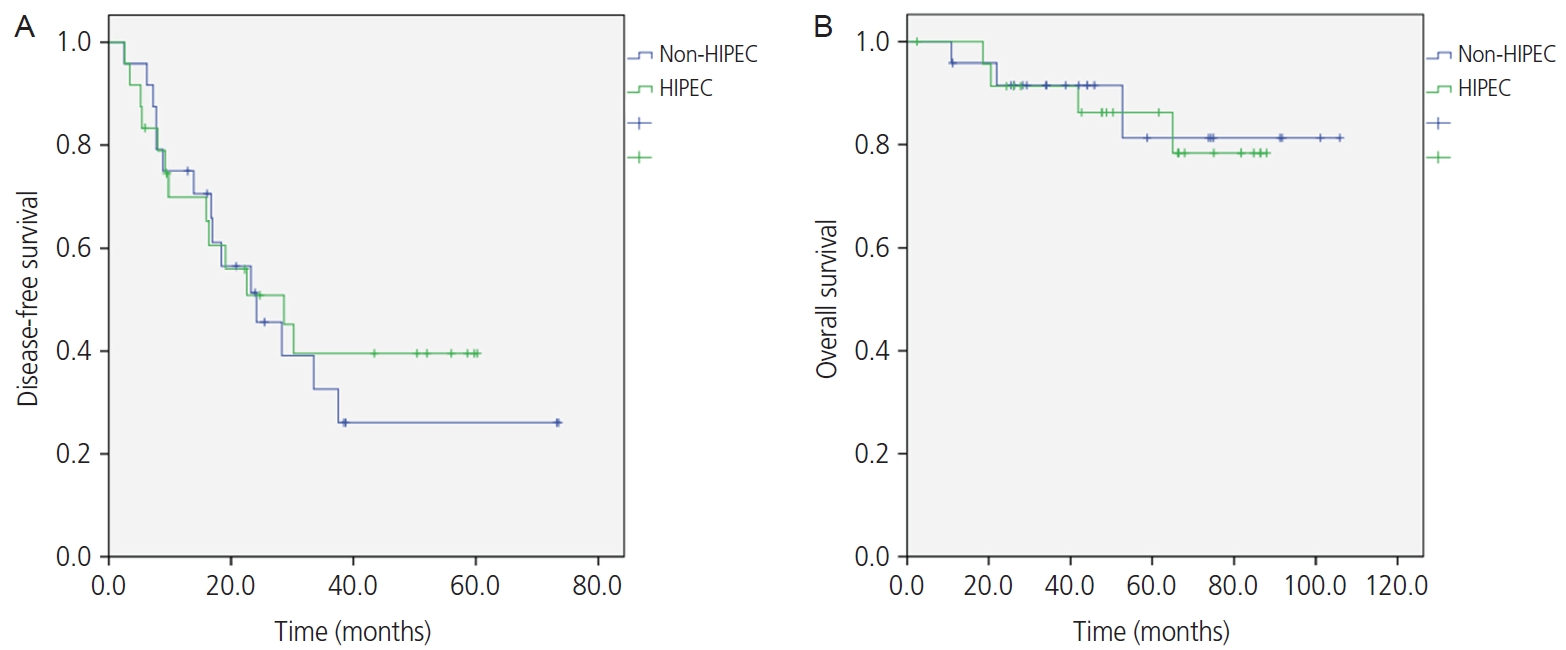
Disease-free survival curve for the patients either treated with consolidation hyperthermic intraperitoneal chemotherapy (HIPEC) or cytoreductive surgery (CRS) and intravenous (IV) chemotherapy (A). Overall survival curve for the patlents either treated with consolidation HIPEC or CRS and IV chemotherapy (B).
3. Adverse events
Adverse events after HIPEC were assessed using the Common Terminology Criteria for Adverse Events (CTCAE) ver 5.0. The most common adverse events were fever and thrombocytopenia. Only one patient developed grade 3 neutropenia. All patients recovered after conservative management.
Discussion
Previous studies have shown that intraperitoneal delivery of chemotherapy is associated with a several-fold increase in concentration in the abdominal cavity compared to that measured in the plasma after IV administration. Several randomized clinical trials have shown that IP combined with IV chemotherapy improves the survival rate in women with optimally debulked stage III ovarian cancer compared to that by conventional IV chemotherapy [11]. However, a recent phase III Gynecologic Oncology Group (GOG)-252 trial reported that IP chemotherapy is not beneficial for progression free survival (PFS) when compared to IV chemotherapy [12], although whether the addition of bevacizumab equalized outcomes remains unclear.
Since HIPEC is performed intraoperatively, the drug is administered uniformly under observation and abstracted thereafter. This can maximize the advantage of IP chemotherapy while reducing disadvantages such as pain and systemic toxicity. Although we observed one or more episodes of adverse events for each patient, all were grade one-two except for one episode of grade three neutropenia (absolute neutrophil count [ANC] <1,000 mm3). All patients tolerated and recovered after conservative care.
Various time points can be considered when performing HIPEC for the treatment of ovarian cancer, including upfront CRS, IDS, consolidation surgery, secondary CRS, and salvage CRS [13]. We considered it more effective and feasible to perform HIPEC as a consolidation treatment rather than performing primary debulking surgery because of tumor burden, operation time, and postoperative morbidity. In addition, lysis of postoperative adhesions before HIPEC application may increase the permeability of chemotherapy.
A randomized trial published by Spiliotis et al. [14] found a 13-month improvement in survival with the addition of HIPEC to secondary CRS, a benefit found in both platinumsensitive and platinum-resistant cohorts. More recently, van Driel et al.’s [9] randomized study on patients with stage III ovarian cancer undergoing neoadjuvant chemotherapy and IDS with or without HIPEC demonstrated similar results as previously described. Women who underwent IDS with HIPEC demonstrated a 3.5-and 12-month improvement in PFS and OS, respectively.
Meanwhile, reports evaluating HIPEC for consolidation purposes have been limited. Bae et al. [15] retrospectively compared the survival rates of patients with ovarian cancer who underwent second-look surgery plus HIPEC with paclitaxel (n=22) or carboplatin (n=45) to no second-look surgery (conventional treatment, n=29). In stage III disease, the 3-year PFS rates were 56.3% and 16.7% in the HIPEC and control groups, respectively (P=0.0028). In another retrospective matched-control study, Mendivil et al. [16] compared the survival rates of patients with advanced-stage ovarian cancer who were treated with consolidation HIPEC with carboplatin (n=69) or not (n=69). They showed more significant benefits of PFS in the HIPEC group (25.1 months) over that in the control group (20 months) (P=0.024) although not shown in OS (P=0.29). A study conducted by Gori et al. [17] reported that patients treated with IP hyperthermic perfusion as consolidation therapy showed a median survival of 64.4 months, whereas the control group showed 60.1 months (P=0.598). The mortality rate was lower in the intraperitoneal chemotherapy (IPCT)+hyperthermia (HT) group (44.8% vs. 57.9%), but the differences were not statistically significant.
No statistically significant survival benefit was observed in the consolidation HIPEC group in this study. The median DFS was 28.7 vs. 24.2 months in the HIPEC and non-HIPEC groups, respectively (P=0.688). Moreover, the 3-year DFS rates in the HIPEC and non-HPEC groups were 39.5% and 32.6%, respectively. The 5-year OS rates in the HIPEC and non-HIPEC groups were 86.2% and 81.3%, respectively (P=0.850) (Fig. 1). This may be due to limitations associated with retrospective studies with a small number of patients, and several differences in methodology and chemotherapy agents used in previous studies.
This study has some limitations. Several prognostic factors other than HIPEC may affect survival rate and should be considered. Age was an important prognostic factor. The patients in the HIPEC group were 6.7 years younger than those in the non-HIPEC group in our study (49.2 years vs. 55.9 years; Table 1). This could be a result of the reluctance to perform HIPEC in relatively elderly patients during the study period. This can also be a limitation of the retrospective comparative studies. Approximately 41.7% (10/24) of patients in the HIPEC group received further maintenance chemotherapy for positive pathologic results after HIPEC, although a previous study suggested that three cycles of consolidation chemotherapy with paclitaxel and carboplatin might not prolong the survival rate in advanced ovarian cancer patients [18]. Although no statistical difference was observed, the use of target agents, such as bevacizumab [19] or PARP inhibitors [20], and BRCA status [21] (Table 1) may also have influenced the prognosis. Moreover, second-look surgery for consolidation is not currently accepted as a therapeutic strategy for advanced ovarian cancer. However, this surgery should be performed for the consolidation process of HIPEC, although it may be unnecessary.
According to the results of this study, no severe specific safety issues or survival benefits were found in HIPEC consolidation. Furthermore, there is a burden that patients must undergo unnecessary second-look surgery to perform HIPEC consolidation. Therefore, we could not routinely recommend HIPEC consolidation for patients with advanced-stage ovarian cancer, particularly outside of an approved clinical trial.
Several ongoing randomized trials have evaluated the benefits of HIPEC use in primary and recurrent ovarian cancer [22,23]. To date, most successes with HIPEC have been observed when used during IDS, and ongoing trials are examining the optimal timing of HIPEC application. These studies provide useful information about this therapeutic strategy.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
This study was approved by the institutional review board (CHA IRB 2018-11-049). The study was performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
Written informed consent and the use of images from patients are not required for the publication.
Funding information
None.

