The ON-Q pain management system in elective gynecology oncologic surgery: Management of postoperative surgical site pain compared to intravenous patient-controlled analgesia
Article information
Abstract
Objective
The goal of this study was to compare postoperative surgical site pain in gynecologic cancer patients who underwent elective extended lower midline laparotomy and managed their pain with either the ON-Q pain management system (surgical incision site pain relief system, ON-Q pump) or an intravenous patient-controlled analgesia pump (IV PCA).
Methods
Twenty gynecologic cancer patients who underwent elective extended lower midline laparotomy were divided into two groups. One group received a 72-hour continuous wound perfusion of the local anesthetic ropivacaine (0.5%, study group) into the supraperitoneal layer of the abdominal incision through the ON-Q pump. The other group received intravenous infusion pump of patient-controlled analgesia (fentanyl citrate 20 mg/mL · kg+ondansetron hydrochloride 16 mg/8 mL+normal saline). Postoperative pain was assessed immediately and at 6, 24, 48, 72, and 96 hours after surgery using the visual analogue scale.
Results
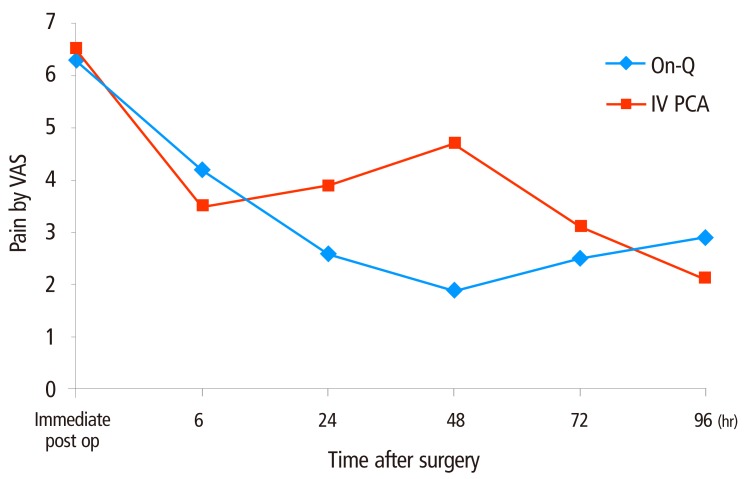
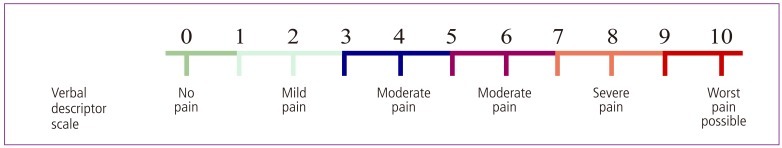
Postoperative surgical site pain scores at 24, 48, and 72 hours after surgery were lower in the ON-Q group than the IV PCA group. Pain scores at 24 hours and 48 hours after surgery were significantly different between the two groups (P=0.023, P<0.001). Overall painkiller administration was higher in the ON-Q group but this difference was not statistically significant (5.1 vs. 4.3, P=0.481).
Conclusion
This study revealed that the ON-Q pain management system is a more effective approach than IV PCA for acute postoperative surgical site pain relief after extended lower midline laparotomy in gynecologic cancer patients.
Introduction
Surgery is a major stressor that induces secretion of various substances such as prostaglandin, serotonin, and histamine as a reaction to localized tissue damage. In laparotomies with larger incisions, intra-abdominal surgical incision site pain is the most significant cause of acute postoperative pain. Extended lower midline laparotomies have relatively long incisions, and thus effective pain control of the surgical incision site is particularly important. Pain at the intra-abdominal incision site which is not effectively controlled interferes with the deep breathing necessary for early ambulation and recovery from atelectasis. Uncontrolled pain can also affect the respiratory, cardiovascular, digestive, urinary and musculoskeletal system, thereby making it difficult to recover quickly from surgery, as well as affecting the overall success of the surgery. Various methods including epidural anesthesia, intraspinal anesthesia, intrapleural anesthesia, and intravenous patient controlled analgesia are used to control postoperative pain, and parenteral narcotics are commonly used as anesthesia. Even though parenteral narcotics play a key role in the reduction of postoperative pain, they include many side effects such as nausea, vomiting, an itching sensation, palpitation, low blood pressure, weakening of muscles, and dizziness. Other serious side effects include difficult urinating, paralytic ileus, miosis, increased intracranial pressure and respiratory suppression. There have been many attempts to reduce these side effects, such as combining parenteral narcotics with other drugs or adjusting the dose of narcotic analgesia, but some side effects still persist.
Continuous injection of local analgesia into the surgical incision site has been effectively used to reduce the side effects of narcotics [1-16]. The ON-Q pain management system (ON-Q PainBuster, referred to as ON-Q pump) created by the I Flow Corp. (Lake Forest, CA, USA) is a device that continuously administers local analgesia directly into the intra-abdominal surgical wound site. Studies comparing the use of this device to a placebo have been carried out over the past several years in numerous surgical departments [4,17-19]. However, no study has evaluated postoperative surgical incision site pain control using the ON-Q pump in gynecologic cancer patients who underwent oncologic surgeries with an extended lower midline incision.
This study randomly selected gynecologic cancer patients who had undergone oncologic surgeries with an extended lower midline incision, and compared postoperative intra-abdominal surgical incision site pain between a group that administered local analgesia directly into the incision site wound by ON-Q infusion pump, and a group that administered parenteral narcotics via intravenous patient-controlled analgesia (referred to as IV PCA).
Materials And Methods
Gynecology oncologic patients who completed baseline studies with a confirmed diagnosis of carcinoma between November 2011 and April 2012 at the Department of Obstetrics and Gynecology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea were selected as study subjects. Twenty patients consented to use a pain control device following gynecology oncologic surgery and were randomly divided into two groups of ten. Postoperative intra-abdominal surgical incision site pain was compared between the group that administered local analgesia through an ON-Q pump (ON-Q pain management system, I Flow Corp.) inserted into the surgical incision site, and the group that administered parenteral narcotics via IV PCA. The groups consisted of patients who underwent laparotomy through a lower midline incision that extended 6 to 7 cm above the umbilicus from the pubic bone. Surgeries were limited to the staging operation, including total abdominal hysterectomy (or radical abdominal hysterectomy) and bilateral pelvic lymph node dissection, but could be modified by each diagnosis. Patients who received an American Society of Anesthesiologist grade of more than IV; had an allergic reaction to ropivacaine hydrochloride, fentanyl citrate or ketorolac tromethamine; had a history of drug or alcohol addiction in the last six months; or had serum creatinine levels greater than 2 mg/dL were excluded from this study.
A multifilament synthetic absorbable suture was used for closure from the peritoneum to the subcutaneous layer, and a disposable skin stapler with a width of 9.9 mm was used to suture the skin. All surgeries and insertion of the ON-Q pump catheter were performed by the same surgeon and surgical assistants using standard surgical procedures.
Age, body mass index (BMI), duration of surgery, length of incision, duration of hospitalization following surgery, final diagnosis, old scar revisions, name of operation, postoperative surgical incision site pain score at each point, and the number of times postoperative analgesia was administered were all noted in electronic medical records. The visual analogue scale (VAS) was used to assess pain (Fig. 1). VAS provides a simple, minimally intrusive measure of pain intensity that has been widely utilized in research settings that require a quick and quantitative pain index. VAS consists of a 10-cm horizontal line with two endpoints labeled as "no pain" and "the worst possible pain." The distance (in centimeters) from the low end point of VAS to the patient's mark is considered a numerical index of pain intensity. The patients used the VAS to report a postoperative pain score at the intra-abdominal surgical incision site immediately following surgery, as well as 6, 24, 48, 72, and 96 hours after surgery. During surgery, both groups received 20 µg/mL of remifentanil at an average rate of 10 mL/hr. For the ON-Q group, 50 µg/mL of fentanyl citrate was intravenously injected once at the end of surgery. For the IV PCA administered group, no additional analgesia was provided at the end of the surgery. Both groups controlled additional pain only with an intravenous injection of ketorolac tromethamine (30 mg/mL) at the patients' request. When the patients started ingesting soft diet, oral nonsteroidal anti-inflammatory drugs (NSAIDs) were given three times daily.
Visual analogue scale (VAS): The VAS provides a simple and efficient measure of pain intensity that has been used widely and consists of a 10 cm horizontal line with the two endpoints labeled as "no pain" and "worst pain." The distance (centimeters) between the low end of the VAS and the patient's mark is used as a numerical index of pain intensity.
1. ON-Q pain management system
The ON-Q pain management system includes an elastomeric pump filled with local analgesia solution (total volume of 300 mL), which is a mixture of 400 mg of ropivacaine hydrochloride (Nacaine [Huons] 40 mg/20 mL) and 100 mL of 0.9% normal saline. This elastomeric pump is connected to a catheter inserted into the intra-abdominal surgical incision site, and is designed to inject 300 mL of 0.5% ropivacaine solution through two strands of soaker catheter at the rate of 2 mL/hr each for 72 hours with consistent pressure (10 psi) (Fig. 2).

Elastometric pump filled with local anesthetic. The protective cap is first removed from the pump, a syringe filled with local anesthetic is attached to the fill port, and the fluid is injected into the pump.
Soaker catheters were placed by inserting 20-gauge guiding needles into the subfascial supraperitoneal layer of the surgical incision after having sutured up to the peritoneum. The guiding needles were placed about 3 cm from the midline incision at the upper and lower position of the incision line. Once the introducer was fixed in the desired location, the needle was removed and a length of catheter approximately 6 to 10 cm was embedded in the incisional wound prior to suturing the skin. When both upper and lower catheters were fixed securely, a bolus of ropivacaine (10 mg/5 mL) was injected through both strands of soaker catheters and the ON-Q infusion pump was connected immediately. The pump contents were then continuously infused into the surgical incision site at a flow rate of 4 mL/hr (2 mL/hr per catheter) for 72 hours. The catheters located in the subfascial supraperitoneal layer were so thin that no subcutaneous suture was necessary, although fixed dressing of catheters was necessary at the injection site. An extra 20 mg/10 mL of ropivacaine was injected directly into the subcutaneous layer prior to suturing the skin (Fig. 3).
2. Intravenous patient-controlled analgesia
Before surgery was completed, IV PCA was initiated via intravenous infusion (Accufuser Plus) with a total of 100 mL of mixed solution of fentanyl citrate (20 mg/mL per kg) and ondansetron hydrochloride (16 mg/8 mL) in 0.9% normal saline, which is the standard solution at the study institution. Although IV PCA was infused continuously at the basic flow rate of 2 mL/hr, 0.5 mL of bolus can be injected if the patients press the button once upon experiencing pain. The lock-out time for each bolus injection was 15 minutes.
For statistical analysis, a descriptive analysis was carried out first. The Mann-Whitney U test was used to examine differences in continuous variables between the groups, and Fisher's exact chi-square test was utilized to examine differences in nominal variables between groups. P-values less than 0.05 was considered statistically significant. Statistical analyses were performed with PASW statistics ver. 18.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Among the 20 patients that participated in this study, ten were in the ON-Q group and ten were in the IV PCA group. No patients stopped taking medication due to side effects or for other reasons, although two patients in the IV PCA administered group had to temporarily stop medication due to nausea and dizziness in the middle of administration on the day of surgery. In these cases, medication was resumed within several hours once the side effects were controlled by allopathic medication, and ultimately the complete dosage of IV PCA was dispensed.
Table 1 summarizes the basic characteristics of each analgesia group including age, BMI, duration of surgery, length of incision, duration of hospitalization, final diagnosis, whether or not old scars were revised, and name of operation. The average age of the ON-Q and IV PCA groups were 56.2 ±8.2 years and 50.8 ±8.2 years, respectively. The average length of incision for the ON-Q group was longer than that of the IV PCA group (25.3±1.2 cm vs. 24.7±1.1 cm). Differences in age and incision length were not statistically significant. There was also no statistically significant difference between the ON-Q group and the IV PCA group in terms of BMI, duration of surgery, duration of hospitalization, and whether or not old scar revision was performed. Two patients in the ON-Q group and three patients in the IV PCA group underwent surgery following a diagnosis of uterine cervical cancer, and two patients in the ON-Q group and three patients in the IV PCA group underwent surgery following a diagnosis of endometrial cancer. One patient in the ON-Q group was diagnosed with recurrent ovarian cancer and underwent a debulking operation including total abdominal hysterectomy and lymphadenectomy at this study institution, followed by bilateral salpingo-oophorectomy at other institution. There were no statistically significant differences between the groups in terms of final diagnosis and surgeries that were performed (Table 1).
The average postoperative pain score at the surgical incision site in the ON-Q group was lower than the IV PCA group immediately after surgery, as well as 24, 48, and 72 hours after surgery (Table 2), although the differences were statistically significant only at 24 hours and 48 hours (24 hours, P=0.023; 48 hours, P<0.001). This suggests that the intra-abdominal surgical incision site was less painful in the ON-Q group during the postoperative acute phase. On the other hand, the average pain score 96 hours after surgery was significantly higher in the ON-Q group (2.9±0.9) than the IV PCA group (2.1±0.6) (P=0.035) (Fig. 4). The number of times painkiller administered additional postoperative analgesia was higher in the ON-Q group (5.1±3.4) than that in the IV PCA group (4.3±3.3), although this difference was not statistically significant (P=0.481).
Discussion
Local analgesia is a relatively safe and inexpensive painkiller that controls pain by blocking the transmission of pain from peripheral nerves at the damaged site. However, the use of local analgesia is limited and frequent re-administration is necessary due to the relatively short analgesic effect, which is 2 to 6 hours on average for single dose. The ON-Q pump created by I Flow resolves the issue of repetitive administration and efficiently blocks the transmission of pain from the surgical incision site to the spinal cord via a continuous infusion system [20-25]. Wound perfusion with local anesthetic solution by an indwelling irrigation unit was first designed by Capelle [26] in the 1930's. In the 1950's, Blades and Ford [27] refined this technique for thoracotomy incisions with the insertion of a fine catheter before closure, and noticed an associated decrease in opioid requirements. Additional research on upper abdominal wounds confirmed a decrease in opioid requirements. Nevertheless, this technique did not achieve popularity at that time. It did, however, begin to receive attention as a 'new method of pain relief' when re-discovered by Samarji [28] in 1972 [29,30]. The ON-Q pump, which provides a continuous infusion of local analgesia into the surgical incision, has proven to be an effective method of managing postoperative pain and reducing the use of opioids in a wide range of medical fields including general surgery, urology, and thoracic surgery [31-39]. Fredman et al. [17] and Givens et al. [18] evaluated the effect of the ON-Q pump on pain reduction and opioid use in obstetric patients after caesarian section. They demonstrated the importance of maintaining blood levels of unbound ropivacaine below the toxic threshold by comparing a group using local anesthetics with a placebo group using normal saline. Gupta et al. [19] showed that application of the ON-Q pump provides more effective postoperative pain relief for total abdominal hysterectomy than a placebo, while Zimberg et al. [40] revealed that the ON-Q pump can reduce the duration of hospitalization following total abdominal hysterectomy, thereby cutting hospital costs up to 30%.
IV PCA is the most commonly used method in postoperative pain control for patients undergoing gynecology oncologic surgery with an extended midline incision. However, this study found that the ON-Q pump was more helpful in pain control at the surgical incision site during the postoperative acute phase, and was significantly more effective at 24 hours and 48 hours after surgery (P=0.023, P<0.001, respectively). Pain scores at the surgical incision site decreased as time passed after surgery in both the ON-Q group and the IV PCA group, whereas the pain score increased at 96 hours after surgery in both groups. This finding at 96 hours after surgery suggests less meaningful because both ON-Q and IV PCA had already been dispensed at this point. In terms of the number of times a patient administered additional analgesia, on average the ON-Q group administered analgesia more frequently than the IV PCA group (5.1±3.4 vs. 4.3 ±3.3, respectively). The autonomic nerve system including the inferior hypogastric nerve plexus can be damaged by a wide transection of the uterosacral ligament, particularly in radical abdominal hysterectomy, and is known as one of the main factors in immediate postoperative pain [41,42]. This study only considered postoperative pain at the surgical incision site and excluded visceral pain such as the pain described above, or musculoskeletal pain due to the long operating time. Considering the difference in the number of times of analgesic was administered between the two groups was less than 1.0, pain score errors associated with the relief of visceral or musculoskeletal pain should be negligibly small. The average period of hospitalization was longer in the ON-Q group (9.9 ±3.7 days) than in the IV PCA group (9.2 ±3.0 days) (P=0.796), but the median value for duration of hospitalization in the ON-Q group was 8.0 days, which was shorter than the 8.5 days for the IV PCA group. The average duration of hospitalization in the ON-Q group seems to be skewed by one patient in the ON-Q group who was discharged on the day 19 after finishing the first postoperative adjuvant chemotherapy on day 14 following the staging operation. While two patients in the IV PCA group temporarily stopped administration of IV PCA due to nausea and dizziness, the ON-Q group did not have any side effects or any cessation during administration. Thus the ON-Q pump was able to substantially reduce the need for additional drugs such as anti-emetics.
This study differs from previous ON-Q pump studies in that it compares the effect of the ON-Q pump with IV PCA instead of a placebo. IV PCA is generally administered in gynecology oncologic laparotomies and has limited use during the postoperative acute phase due to various side effects of narcotics. However, if there are minimal side effects, IV PCA can be used in accordance with additional medication such as antiemetics.
Hypersensitivity is a known side effect of the ON-Q pump and is caused by the ester series of anesthetics, but it is very rare and occurs in less than 1% of patients using the ON-Q pump [43]. Because ON-Q pump catheters are embedded in the incisional wound during the operation, it is possible to reduce unnecessary medication without generalized side effects or additional pain. Moreover, by relieving pain in the surgical wound area, which is the main cause of postoperative pain in the acute phase, the ON-Q pump helps prevent pulmonary complications such as atelectasis and aids in early ambulation and early recovery of bowel movements in gynecology oncologic surgeries with a long incision, all without the use of IV PCA. Consequently, the ON-Q pump is highly beneficial to cancer patients who desire a quick recovery from surgery for postoperative adjuvant anti-cancer therapy.
This study shows that acute postoperative surgical incision site pain is well controlled using only the ON-Q pump and additional intravenous NSAIDs, without opioid-based IV PCA, after laparotomy of gynecologic cancer with an extended lower midline incision. However, this study had a small sample size which made it difficult to use a linear regression model to determine whether the use of additional pain relievers or the average period of hospitalization was affected by parameters other than the method of postoperative pain control. Therefore, future studies should use a larger sample size and should evaluate the effect of the ON-Q pump on generalized pain such as visceral and musculoskeletal pain. In addition, future studies should specify indices of early recovery and establish a multi-regimen protocol for postoperative pain control.