Outcomes of ‘one-day trial of vaginal delivery of twins’ at 36–37 weeks' gestation in Japan
Article information
Abstract
Objective
The lack of obstetricians in Japan has prevented the implementation of a 24–hour delivery monitoring system for high-risk deliveries such as twin vaginal delivery at many obstetric facilities. To examine the outcomes of a 1-day trial of the vaginal delivery of twins at 36–37 weeks' gestation.
Methods
We induced the vaginal delivery of twins at 36–37 weeks' gestation of 256 women who provided consent between January 2007 and December 2016 using the following protocol: 1) administration of 0.5 mg oral prostaglandin E2 every 1 hour (maximum: 1.5 mg) in the morning; 2) intravenous administration of oxytocin and amniotomy in the afternoon; and 3) selection of caesarean delivery when vaginal delivery was not expected by evening. We examined their perinatal outcomes in a chart review.
Results
The completion rates of vaginal delivery in total, nulliparous, and multiparous women were 79%, 72%, and 84%, respectively. There were no cases of neonatal asphyxia. The total incidence of neonatal respiratory disorders was 2.1%, but there were no cases of persistent pulmonary hypertension. The total incidence of postpartum hemorrhage requiring transfusion was 2.7%.
Conclusion
The 1-day planned vaginal delivery of twins at 36–37 weeks' gestation appears valid and safe, and our findings suggest that it can be an option for the delivery of twins.
Introduction
If the delivery monitoring and neonatal resuscitation systems are in place, for twin gestations with a cephalic-presenting first twin, planned vaginal delivery at 35–38 weeks' gestation in selected women has been recognized as a safe option, especially in centers equipped to actively manage the second twin delivery [123456]. Rather, in twin pregnancies, some reports pointed out the risk of severe acute maternal morbidity after planned cesarean delivery in women older than 35 years or postpartum hemorrhage in vaginal delivery at ≥39 weeks' gestation [78].
In Japan, however, the lack of obstetricians caused by a poor work environment and increasing medical lawsuits have prevented the implementation of a strict 24-hour delivery monitoring system at many obstetric facilities [910]. For example, although our institute is one of the 29 major perinatal centers in Tokyo, Japan (about 1,900–2,100 deliveries per year), only 1–2 obstetricians are routinely on staff overnight (5:20 PM to 8:20 AM). Therefore, in our institute, high-risk deliveries such as twin deliveries are scheduled to occur during daytime hours, when 2–4 obstetricians are available. We understand that the safety of the delivery method should be ensured. Therefore, here we examined the outcomes of the planned vaginal delivery of twins in a single day, i.e., 1-day trial of vaginal delivery of twins.
Materials and methods
We reviewed the obstetric records of all twin deliveries beyond 36 weeks' gestation at Japanese Red Cross Katsushika Maternity Hospital between January 2007 and December 2016. Demographic information and the labor and delivery characteristics were extracted from the patient charts. Cases of intrauterine death of one fetus were excluded from this analysis.
Since 2007, we have performed the 1-day trial of vaginal delivery of twins for women with twin pregnancy at 36–37 weeks' gestation. Although 36–37 weeks' gestation may be a little early, they were selected to increase the possibility of planned delivery management. In this study, we examined the perinatal outcomes in the 1-day trial of vaginal delivery of twins to confirm the validity and safety of this approach for nulliparous and multiparous women separately since nulliparity is a recognized risk factor strongly associated with cesarean delivery of twin pregnancies [111213].
In our hospital, the applicable conditions for 1-day trial of vaginal delivery of twins in women without severe complications include: 1) the presence of a maternal request for vaginal delivery with understanding the planned delivery methods (described later); 2) vertex presentation of the first twin; 3) gestational age at delivery at 36–37 weeks' gestation; and 4) estimated birth weight of at least 2,000 g for each twin. During this period, elective cesarean section was performed in cases of a suspected fetoplacental circulation imbalance between the twins, a history of previous cesarean deliveries, or a labor that occurs at an understaffed time of day.
The protocol of 1-day trial of vaginal delivery of twins is as follows: 1) hospitalization at 8:00–9:00 AM on the day the management staff was secured; 2) confirmation of reassuring fetal statuses on the fetal heart rate tracing upon hospital admission; 3) administration of 0.5 mg oral prostaglandin E2 (Prostarmon-E, Osaka, Japan) every 1 hour (maximum: 1.5 mg) from 9:00 to 10:00 AM; 4) intravenous administration of oxytocin at an initial dosage of 1–2 mU/minute from 11:00 AM to 1:00 PM; 5) amniotomy at 1–2 hours after the start of oxytocin; 6) selection of caesarean delivery when vaginal delivery cannot be expected by 5:00–6:00 pm; 7) intravenous administration of bolus doses of oxytocin (5–20 IU) immediately after placental delivery to prevent postpartum hemorrhage; and 8) confirmation of the presence or absence of a retained placenta by ultrasonography. Since there are no full-time anesthesiologists in our institute, obstetricians usually perform spinal anesthesia themselves in cases of emergent cesarean section. In addition, we do not administer epidural anesthesia for vaginal twin deliveries in anticipation of the risk of postpartum hemorrhage.
In this study, we examined maternal age, chorionicity, fetal presentation of the second twin, and fetal growth (birth weight) as additional potential risk factors of emergency cesarean delivery [111213]. As the secondary aims of this study, we examined indications for emergency cesarean section for both twins or the second twin, the expression of neonatal depression (defined by an Apgar score <7 at 1 minute), the presence of neonatal asphyxia (defined by an umbilical artery pH <7.0), and postpartum hemorrhage requiring transfusion. The diagnoses of respiratory distress syndrome (RDS) and transient tachypnea of the newborn (TTN) were made by neonatologists using the clinical and radiology data.
Data are presented as number (%). Statistical analyses were performed SAS version 8.02 (SAS Institute, Cary, NC, USA). Odds ratios (ORs) and 95% confidence intervals (CIs) were also calculated.
Results
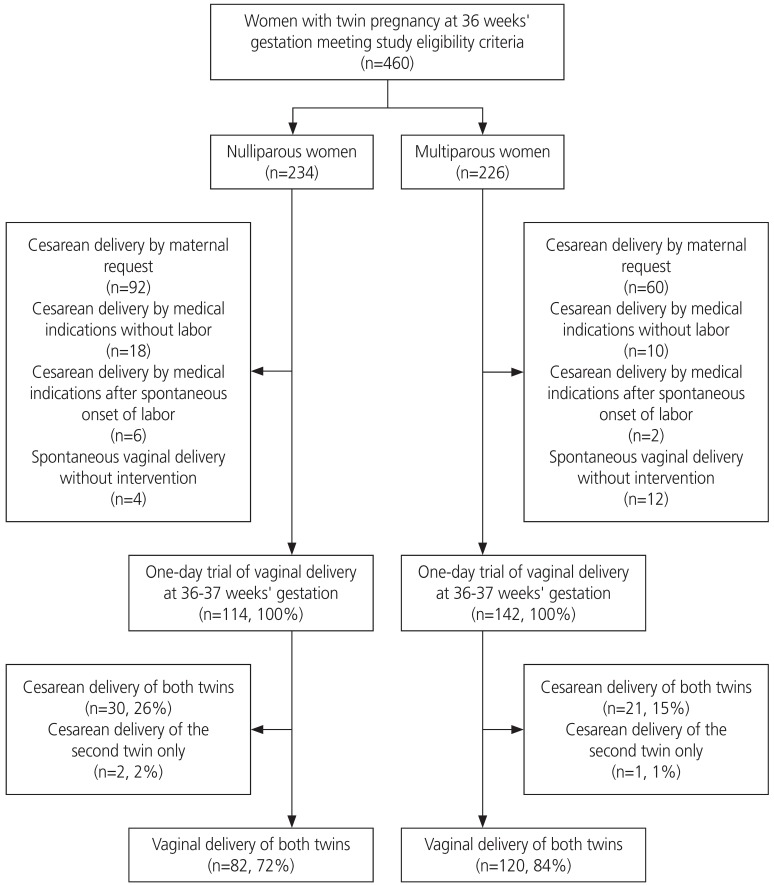
Of the 460 women who met the eligibility criteria during the study period, 114 nulliparous (25%) and 142 multiparous women (31%; total 246 women, 56%) attempted labor. The completion rates of vaginal delivery in total, nulliparous, and multiparous women were 79%, 72%, and 84%, respectively (Fig. 1). The completion rate of vaginal delivery among the multiparous women was statistically higher than that in the nulliparous women (crude OR, 2.13; 95% CI, 1.2–3.9; P=0.02).
Table 1 shows the clinical characteristics of the nulliparous and multiparous women who met the eligibility criteria. There were no statistically significant differences in these valuables between the nulliparous and multiparous women.
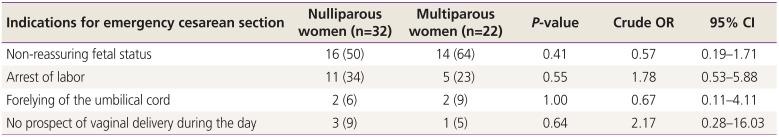
Table 2 shows the indications for emergency cesarean section in women who attempted labor. There were no measurable differences in these indicators between the nulliparous and multiparous women. There was one case of acute twin–twin transfusion syndrome in a monochorionic twin pregnancy with vertex–vertex presentation; however, there were no statistically significant differences in the cesarean rate between monochorionic and dichorionic twin pregnancies (crude OR, 1.28; 95% CI, 0.69–2.4; P=0.43) or between vertex and non-vertex presentation of the second twin (crude OR, 1.79; 95% CI, 0.80–4.0; P=0.20).

Indications for emergency cesarean section in women underwent ‘one-day trial of vaginal delivery of twins’ at 36–37 weeks' gestation
Table 3 shows the perinatal outcomes of this study. Although the rate of neonatal depression in the second twin was higher than that in the first twin (crude OR, 10.5; 95% CI, 1.7–64, P<0.01); however, there were no cases of neonatal asphyxia in this study population. The total incidence of RDS/TTN was 2.1% (11/512). There were no statistically significant differences in the incidence of RDS/TTN between the first and second twins (crude OR, 2.77; 95% CI, 0.55–5.7; P=0.54). Of them, there were no cases of persistent pulmonary hypertension. The total incidence of postpartum hemorrhage requiring transfusion was 2.7% (9/256). There were no statistically significant differences in these variables between the nulliparous and multiparous women (Table 3).
Discussion
The rate of emergency cesarean delivery rate of our 1-day trial of vaginal delivery of twins at 36–37 weeks' gestation was 21% (54/254). The rate seemed to be lower than or similar to those observed in some previous studies [12345]. We were concerned that our attempt with time constraints had decreased the possibility of vaginal deliveries in women with twin pregnancies; however, we are pleased with the high completion rate of vaginal delivery of twins in our aggressive trial under time constraints. In this study, there were no cases of neonatal asphyxia defined by an umbilical artery pH <7.0 or persistent pulmonary hypertension in the neonates. Compared with some previous studies, in addition, the incidence of neonatal respiratory disorders did not seem high [1415]. These can support the validity and safety of our protocols for vaginal delivery of twins.
In some previous studies [1617], twin gestations were observed to have a significantly shorter first stage of labor than singleton gestations. For example, Schiff et al. [17] observed that twin gestations in nulliparous women have a shorter first stage of labor than their matched singleton control gestations (average, 3.0 vs. 4.0 hours; P<0.01). In addition, twin gestations had no adverse impact on the effectiveness or efficiency of oxytocin labor stimulation [18]. In this study, the rate of cases with no prospect of vaginal delivery during the day of our protocol's use was 2% (4/256); therefore, a long time may not be required to complete the vaginal delivery of twins. In addition, the completion rate of vaginal delivery of the multiparous women was significantly higher than that of the nulliparous women. This may also support some previous studies indicating that women who deliver vaginally are more likely to be multiparous associated with a high advanced cervix at admission [1319]. Under the current time-limited protocols, the trend may have been stronger.
In the current study, the incidence of neonatal depression in the second twin was higher than that in the first twin, although there were no cases of neonatal asphyxia. A recent study by Algeri et al. [20] observed that intertwin delivery time is not an influential factor of adverse neonatal outcomes. This may be true in all vaginal deliveries of twins [6212223]. However, in cases of non-reassuring fetal status and/or non-vertex presentation in the second twin, obstetricians have been recommended to be skilled enough to perform a rapid delivery if necessary using internal maneuvers to avoid unnecessary cesarean section to deliver the second twin [6212223]. The current results may also support the previous observations. In addition, because it is necessary to prepare for the rapid delivery of the second twin at any time when attempting a vaginal delivery of twins, the current protocols for twin delivery may also be an acceptable and safe option.
In this study, the incidence of postpartum hemorrhage requiring transfusion did not seem high under our protocols [24]. This may support our recent speculation that the increased risk of postpartum hemorrhage is related to elective cesarean delivery rather than vaginal delivery or emergency cesarean delivery during labor [2526]. The mechanisms leading to increased blood loss after twin delivery were suggested to be associated with primary uterine atony without contraction [26]. The absence of maternal fatigue due to the time limitation may also contribute to the current results. In addition, the intravenous administration of bolus doses of oxytocin and ultrasonographic confirmation in our protocols might have also prevented primary and secondary uterine atony [27]. Therefore, we suggest that the presentation of convincing mechanisms is required for physician counseling to select the twin delivery mode.
In conclusion, the planned vaginal delivery of twins at 36–37 weeks' gestation limited to 1 day seems valid and safe, and our findings suggest that it may be an option for the delivery of twins.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
Ethical approval: The protocol for this analysis was approved by the Ethics Committee of the Japanese Red Cross Katsushika Maternity Hospital (approval No. K2017-021).
Patient consent: Written informed consent for the analysis of their data from a retrospective database was obtained from each subject during the hospital visit.