Incarceration of early gravid uterus with adenomyosis and myoma: report of two patients managed with uterine reduction
Article information
Abstract
Although gravid uterine incarceration is typically diagnosed during the early second trimester, we encountered two unusual cases in early pregnancy. A 34-year-old multiparous woman with adenomyosis presented at 7 + 2 weeks of gestation with increased urinary frequency and a sensation of incomplete bladder emptying. The uterine incarceration was successfully reduced by manual reduction and pessary insertion, and she delivered a normal infant at term. In the second case, a 31-year-old nulliparous woman with a large myoma complained of dysuria, acute urinary retention, and intense back pain at 6 weeks of gestation. Manual reduction was successful in the knee-chest position. Subsequent pessary insertion failed; however, a slight reduction in pain was achieved. After a week, the fetus spontaneously aborted. In summary, gravid uterine incarceration is a rare but potentially fatal condition for the fetus, and a suspicion of this condition in patients with urinary symptoms, especially urinary retention and pelvic pain, is important in the early gestation period.
Introduction
Uterine incarceration, defined as intrapelvic locking of the uterine fundus during pregnancy [1], occurs in approximately 1 out of 3,000 pregnancies [2]. As the pregnancy progresses, the myometrium of the incarcerated uterus expands by stretching or sacculation of the anterior uterine wall. During pregnancy, the retroverted uterus rises and grows in the pelvis to accommodate the growing fetus before mid-gestation. If the uterus does not ascend into the abdominal cavity, the fundus becomes entrapped below the sacral promontory and gets fixed in the pelvic cavity, where it continues to enlarge, consequently inverting the polarity of the uterus [3]. Subsequently, the bladder and cervix are pulled up into the abdominal cavity toward the head, and the cervix is elongated and anteriorly displaced behind the pubic symphysis. There are several risk factors for uterine incarceration, including benign uterine tumors such as uterine fibroids and adenomyosis, endometriosis, pelvic adhesive diseases caused by previous pelvic surgery, pelvic inflammatory disease, peritonitis, and abnormal uterine morphology [4].
Although uterine incarceration is rare, if left untreated, it may lead to maternal symptoms, fetal compromise, or complications during cesarean delivery. It may cause not only preterm labor (PTL) or delivery and premature rupture of membranes (PPROM) but also maternal lower abdominal or back pain; vaginal bleeding; rectal pressure; tenesmus; constipation; bladder or uterine rupture; and urinary symptoms such as dysuria, urinary frequency, urinary retention, overflow incontinence, and urinary stasis [567].
A diagnosis of uterine incarceration can be made on the basis of clinical symptoms and physical examination. Common presentations include pelvic discomfort, urinary symptoms including retention and frequency, and gastrointestinal symptoms. Incarceration could be suspected when the cervix is not visualized or palpable, the uterine fundus is at a low level, or a mass fills the cul-de-sac on vaginal examination [4]. Sonography or magnetic resonance imaging (MRI) could help for the diagnosis of uterine incarceration and its treatment. Imaging may aid in the diagnosis of patients with asymptomatic or nonspecific abdominal symptoms [8]. Early diagnosis of uterine incarceration ensures prompt management and can reduce maternal and fetal complications. We describe two unusual cases of early pregnancy with urinary retention. The patients consented to the use of their medical records for research purposes.
Case report
1. Case 1
A 34-year-old multiparous woman was admitted at 7.2 weeks of gestation with acute urinary retention and a mass in the upper vaginal wall. She had adenomyosis (uterus size, 10.4 cm × 11.6 cm), and a 2-week history of increased urinary frequency and a sensation of incomplete bladder emptying. In the emergency room, 850 mL of urine was drained by urinary catheterization. Transvaginal (TV) ultrasound and MRI showed no specific findings except a retroverted gravid uterus with adenomyosis, and an elongated and anteriorly displaced cervix behind the pubic symphysis (Fig. 1A; TV ultrasound, Fig. 1C; MRI). Nonetheless, uterine incarceration was clinically suspected. The change in uterine polarity was noted after manual reduction (Fig. 1B), and a pessary was inserted to prevent recurrence (74 mm; Smiths Medical, Minneapolis, MN, USA). The pessary was removed at 15 weeks, and the patient delivered a healthy male baby weighing 3,100 g at 38 weeks. Ultrasound examination performed at 6 weeks after delivery showed a retroverted uterus with a slightly thickened wall, although it was thinner than expected (Fig. 1D).
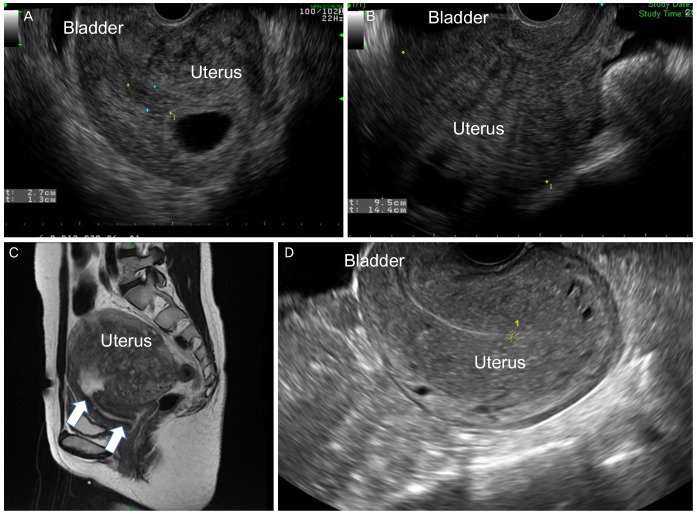
Transvaginal ultrasound demonstrates (A) a retroverted gravid uterus with the gestational sac and; (B) anteverted gravid uterus after manual reduction. (C) Abdominal magnetic resonance imaging shows a retroverted gravid uterus. The cervix is elongated (arrows) and anteriorly displaced behind the pubic symphysis. (D) Retroverted uterus after vaginal delivery at 38 weeks with adenomyosis and a slightly thickened wall.
2. Case 2
A 31-year-old primigravida had been admitted to another hospital for 3 days because of acute urinary retention, which was conservatively managed; the management strategy included pain control. She was referred to us at 6 weeks of gestation, with a 12.6 cm × 9.4 cm-sized myoma in the posterior uterine wall. She also complained of urinary retention and dysuria, along with severe back pain. Pelvic examination revealed fullness in the posterior fornix and anterior displacement of the cervix. On bimanual examination, the retroverted uterine fundus was palpable as a large mass in the cul-de-sac. Ultrasound findings showed the uterus entrapped in the pelvis in the hollow of the sacrum along with a posterior myoma (Fig. 2A). An indwelling urinary catheter was inserted and 750 mL of urine was drained, with the catheter kept in place.
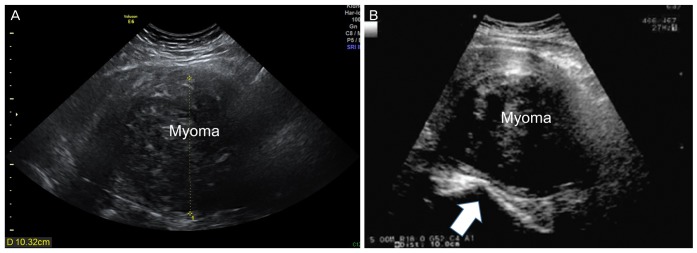
(A) The uterus remained entrapped in the pelvis in the hollow of the sacrum with a posterior myoma. (B) Ultrasonography shows a large myoma after reduction (arrow: sacral promontory).
Manual reduction was attempted by applying steady pressure with two fingers in the posterior vaginal fornix and by pushing the uterus in a cephalad direction without anesthesia while the patient was in the dorsal lithotomy and knee-chest position; however, it failed. Subsequently, gentle bimanual reduction through the rectum and vagina was attempted by applying continuous pressure under ultrasonographic guidance. Subsequently, slight pain reduction was achieved. In order to prevent re-incarceration of the uterus, pessary insertion was attempted; however, it failed owing to the narrow space. Instead, a large gauze was packed in the vagina, the Foley catheter was left in place, and the patient was kept on bed rest for 1 day. Final ultrasound showed a uterine myoma that was positioned slightly upward after reduction (Fig. 2B). On the next day, the gauze and Foley catheter were removed. The patient still complained of intermittent back pain but was able to void the bladder, and was discharged. Although the uterine incarceration improved slightly, the patient subsequently had a spontaneous abortion after 1 week, and a myomectomy was conducted for her subsequent pregnancy.
Discussion
Gravid uterine incarceration is usually diagnosed in the early second trimester, at 14–18 weeks of gestation. In the current cases, uterine incarceration was observed early in the first trimester, at 6–7 weeks of gestation. In addition, Chauleur et al. [9] reported two cases of acute urine retention induced by severe fibroid incarceration at 4 and 5 weeks of gestation, in which the patients visited the hospital presenting with acute urinary retention. After unsuccessful manual reduction in both cases, myomectomy was performed under uterine relaxation.
In the present cases, we attempted to reduce the incarcerated uterus immediately after diagnosis in the symptomatic women. However, most authors in previous studies recommend immediate intervention after diagnosis, even if the patients have no specific symptoms, to prevent adverse maternal and fetal outcomes [10]. The best time for uterine repositioning is from 14 to 20 weeks of gestation. Reduction of the incarcerated uterus is not recommended beyond 20 weeks owing to the risk of PPROM or PTL [11]. Spontaneous reduction can be expected for anterior wall myoma [12]. However, it may be difficult in posterior myoma owing to its easy recurrence [9]. Dierickx et al. [10] stated that as a few rare cases of recurrence of uterine incarceration have been reported, close monitoring with serial ultrasounds should be carried out in subsequent pregnancies.
As stated in the previous case report, and based on our experience, the incarcerated uterus should be managed as follows. Initially, a urinary catheter should be inserted to drain and decompress the bladder. Next, the uterus should be manually reduced by applying gentle pressure with two fingers to the posterior vaginal fornix or rectum, pushing the gravid uterus upward with the patient in the dorsal lithotomy, knee-chest, or Simms position, or under anesthesia. If the abovementioned reduction fails, some other reported methods, namely colonoscopic reduction, could be considered. However, this procedure should be performed by skillful colonoscopists owing to the associated risk of bowel perforation. In some cases, laparoscopy and laparotomy may be required [5913]. Although myomectomy was performed in previously reported cases, it should be carefully planned, as the procedure itself might cause miscarriage. After successful reduction, pessary insertion could be considered to prevent recurrence [10]. Although manual reduction is the first step to manage pregnant women with incarceration, scarce literature is available on the complications of the procedure owing to the uncommon nature of gravid uterine incarceration.
Accurate diagnosis of uterine incarceration is important to ensure proper treatment, as it is a rare disease and is difficult to diagnose. Radiologic examination and the clinical symptoms of the patient could aid the diagnosis. In Case 1 in the present study, ultrasound examination was insufficient to confirm the diagnosis, and the diagnosis was confirmed based on the clinical symptoms of the patient, and the findings of pelvic examination and MRI. Therefore, pregnant women with or without uterine masses including uterine myoma or adenomyosis, and those presenting with urinary retention and pelvic pain, even in early first trimester, should undergo pelvic examination to exclude the possibility of an incarcerated uterus.
The recommended route of delivery is cesarean section if the incarcerated uterus has been detected in the late second trimester or when uterine polarity cannot be corrected [14]. As the bladder of patients with an incarcerated gravid uterus is pulled higher than normal, a uterine incision should be made at a higher position for preventing injury to the bladder, cervix, and vagina [10].
In conclusion, uterine incarceration should be considered even during early gestation in pregnant women complaining of urinary retention and pelvic pain, especially in those with preexisting conditions. Even after reduction, close observation is important to monitor recurrence, and pessary insertion may be helpful in this regard.
Notes
Conflict of interest: No potential conflict of interest relevant to this manuscript was reported.
