Aberrant uterine leiomyomas with extrauterine manifestation: intravenous leiomyomatosis and benign metastasizing leiomyomas
Article information
Abstract
Objective
Intravenous leiomyomatosis (IVL) and benign metastasizing leiomyoma (BML) are uncommon variants of benign uterine leiomyomas with extrauterine manifestations. Categorizing the extent of disease allows clinicians to delineate the clinical spectrum and the level of sophistication for complete surgical resection.
Methods
Twelve patients with IVL and BML were reviewed. They were divided into early versus late stage disease groups, and initial manifestation, clinical characteristics, laboratory values, surgical pathology, and follow up data were summarized.
Results
Patients were mostly pre- or peri-menopausal and parous. Patients with late stage disease were more likely to present with cardiac symptoms or abnormal findings on chest X-ray, whereas those with early stage disease presented with classical leiomyoma symptoms including heavy menstrual bleeding, increased myoma size, or lower abdominal discomfort. Tumor marker levels were within normal ranges. A trend of higher neutrophil to leukocyte ratio was observed in the late versus the early stage group (10.4 vs. 1.51, P=0.07); the platelet leukocyte ratio was statistically higher in patients with late stage IVL (0.23 vs. 0.13, P=0.04). The overall recurrence rate was 25%. No recurrence was observed in stage I or stage III IVL groups, while 50% of the stage II IVL group showed recurrence in the pelvic cavity.
Conclusion
IVL and BML are benign myoma variants with paradoxically metastatic clinical presentation. Careful inquiry of systemic symptoms, the presence of underlying systemic inflammation, and a high index of suspicion are required for preoperative diagnosis. Furthermore, a multidisciplinary approach is necessary to improve outcomes of surgical resection.
Introduction
Intravenous leiomyomatosis (IVL) is an uncommon variant of benign leiomyomas. Unlike classical uterine leiomyomas which are firm, well circumscribed, and localized to the pelvic cavity, IVL clinically manifests as a fragile and malleable leiomyoma that extends through adjacent venous structures in a worm-like fashion [1]. In rare cases, IVL paradoxically manifests as a benign leiomyoma infiltrating into the right heart chamber and the lungs [2]. IVL is difficult to diagnose preoperatively due to the wide range of clinical manifestations, and thus histological differential diagnosis is often required to differentiate IVL from other diagnoses that are categorized together with benign metastasizing leiomyoma (BML) and diffuse peritoneal leiomyomatosis (DPL) under smooth muscle tumors with unusual growth pattern [3]. Despite their extrauterine manifestation, these aberrant of benign leiomyomas are pathologically distinguished from leiomyosarcoma in that sarcoma is marked by mitotic index of greater than 10, high grade cellular atypia, and presence of coagulative tumor cell necrosis [4]. Pathologically, in IVL, benign appearing smooth muscle cells that are found within uterus venous structures show low mitotic activity and stain positively for actin and desmin [5].
BML is characterized by monoclonal proliferation and hematogenous spread of smooth muscle cells from uterine leiomyoma to distant locations, most commonly the lungs [67]. Furthermore, recent investigations involving comparative genetic hybridization, clonal number, and copy variance showed that IVL and BML share the same cytogenetic origin [8]. Histologically, leiomyomas in BML demonstrate strong and diffuse positivity for smooth muscle actin (SMA), estrogen receptor (ER), and progesterone receptor (PR). For both IVL and BML, treatment of choice is total resection of the lesion involved, if possible. Currently there is no consensus on the choice of adjuvant; however, hormonal treatment with progestin, tamoxifen, or a gonadotropin agonist has been suggested [9].
In this study, we encapsulated a single center experience with 10 cases of IVL and 2 cases of BML. All the cases were pathologically confirmed after primary surgery and followed up for adjuvant therapy and disease recurrence. The goal of our study was to review the recent literature in this field and present a series of representative cases in terms of their preoperative clinical characteristics, operative outcomes, and follow up.
Materials and methods
1. Patient enrollment and data collection
We retrospectively reviewed patients diagnosed with IVL and BML at the Severance Hospital from November 2005 to March 2017. Institutional Review Board approval was obtained. Electronic medical records were reviewed to obtain initial symptoms; findings from pre-operative imaging and laboratory studies; operative findings and pathologic features; and follow up information. The primary imaging modality was trans-vaginal ultrasound with the exception of patients with extensive disease, which necessitated other modalities such as pelvic magnetic resonance imaging (MRI), trans-thoracic echocardiography, abdomen or chest computed tomography (CT), and positron emission tomography (PET).
2. Classification of symptoms and clinical manifestation
Based on evaluation prior to primary operation, patients were divided into early stage versus late stage group, following the staging system suggested by Ma et al. [10]. Patients with tumors which have penetrated the uterine venous wall, but were confined to the pelvic cavity, were categorized as stage I. Patients with tumors which have grown into ovarian vein or iliac vein and with extension into abdominal cavity at the level below the renal vein were categorized as stage II. Stage III included patients with extension of tumor through inferior vena cava (IVC) into the right atrium. When tumor progressed to involve the lung parenchyma, patients were classified as stage IV. Initial symptom was classified based on each patient's chief complaint, which included abnormal vaginal bleeding, abdominal pain, mass palpation or abdominal distension, and cardio-pulmonary symptoms such as chest pain and syncope.
3. Statistical analysis
The SPSS statistical software package (SPSS version 23.0; IBM, Chicago, IL, USA) was used for the statistical analysis. The nonparametric (Mann-Whitney U or χ2 tests) and the parametric (Student's t-test) tests were used as appropriate for comparisons. A significance level of 0.05 (P<0.05) was used in all tests.
Results
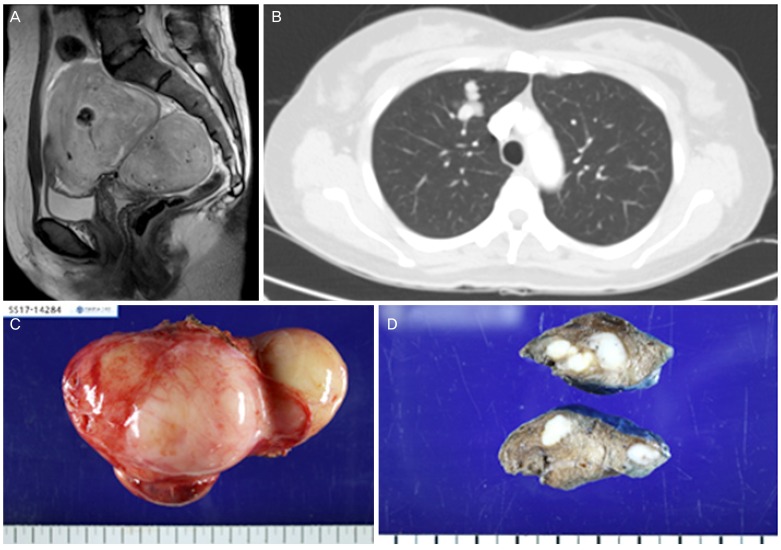
1. Patient characteristics
Out of 35 patients diagnosed with leiomyomatosis, 8 patients with DPL and 15 patients with lymphangioleiomyomatosis were excluded (Fig. 1). A total of 12 patients were included: 10 patients with IVL and 2 patients with BML. All patients were pre-menopausal with median age of 46 years, except for 1 patient who was 60 years old at time of diagnosis (range, 35–60 years). Patients were parous with an average gravida of 4.27. The proportion of those with a history of cesarean section and vaginal delivery were similar. Most patients had a history of dilation and curettage (D&C) procedures (91.7%), whereas only 2 patients had a history of laparoscopic myomectomy (16.6%). The blood and serum laboratory values (mean±standard deviation) are listed in Table 1. Complete blood count showed hemoglobin levels of 11.1±1.72 g/dL, platelet levels of 216±88.7 K/µL, white blood cell count of 6,710±3,077 cells/µL. Serum cancer antigen (CA) 125 and CA19-9 tumor marker levels were 16.0±11.5 U/mL and 3.03±1.21 U/mL, respectively. Calcium (8.7±0.3 mg/dL) and phosphate (3.48±0.53 mg/dL) levels were within normal ranges. The calculated neutrophil leukocyte ratio (NLR) was 7.20±8.09 and the platelet leukocyte ratio (PLR) was 0.19±0.07.

Flowchart of patient enrollment in the study.
DPL, diffuse peritoneal leiomyomatosis; LAM, lymphangioleiomyomatosis; IVL, intravenous leiomyomatosis; BML, benign metastasizing leiomyoma.
Initial manifestations and follow up records are summarized in Table 2. Of the 12 patients, disease extent was limited to the pelvic cavity (stage I) in 4 patients (33.3%), beneath renal vein (stage II) in 4 patients (33.3%), into cardiac chamber (stage III) in 2 patients (16.7%), and to bilateral lungs (stage IV) in 2 patients (16.7%). In total, the most common presenting symptoms were abnormal uterine bleeding (33.3%) and pelvic mass (41.7%). For patients with leiomyoma extension to cardiac chamber, the initial presenting symptoms included chest discomfort and syncope.
To compare the clinical and laboratory values between early and late stage IVL, patients in the early stage IVL (stage I) and late stage IVL (stages II, III, and IV) groups were stratified according to clinical and laboratory values (Table 3). Average age, body mass index, and clinical history such as cesarean section, vaginal delivery, history of D&C procedures, myomectomy, and history of intrauterine device (IUD) usage were not statistically different. Serum creatinine, calcium, phosphate, and albumin levels were not statistically different. NLR of late stage IVL showed a tendency to be higher than that of early stage IVL (10.4 vs. 1.51, P=0.07). PLR of late stage IVL was significantly higher than that of early stage IVL (0.23 vs. 0.13, P=0.04).
Median years of follow up were 5 years. Of the 4 patients diagnosed with stage I IVL, the recurrence rate was 0% after complete resection. In 4 patients diagnosed with stage II IVL, 50.0% of patients had persistent disease or intra pelvic recurrence. Both patients with stage III IVL showed no recurrence in both the pelvic and chest cavity. One of the 2 stage IV IVL patients had persistent disease on follow up. Despite the events of recurrence or persistent disease, there was no operative, hospital, or long-term mortality for the observed period.
2. Case series
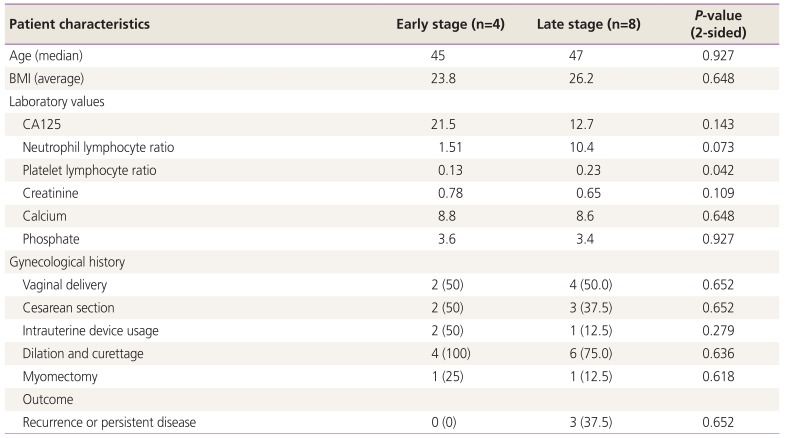
1) Case 1 (stage I, patient #3)
A 46-year-old patient was referred for lower abdominal pain. On sonography, a conglomeration of multiple intramural leiomyomas was detected at the posterior wall of the uterus (Fig. 2). Further evaluation with MRI revealed a 7.4×10 cm sized lobulated subserosal myoma with an internal hemorrhagic area and dilated pelvic and uterine vessels. Uterine sarcoma was proposed as less likely on differential diagnosis. The patient was scheduled to undergo total abdominal hysterectomy (TAH) and bilateral salpingo-oophorectomy (BSO). Frozen section histopathological analysis of tissue from the bulging uterine mass confirmed a leiomyoma with degeneration. The final pathology report showed intravascular leiomyomatosis associated with multiple intramural and subserosal leiomyomas and superficial adenomyosis. Immunohistochemical staining results showed positivity for CD31 and CD34 expression. No adjuvant therapy was used and no recurrence was found after 5 years of follow up.

An example of a stage I, 46-year-old patient with lower abdominal pain. (A) Transvaginal ultrasound showing a conglomeration of multiple intramural myomas and (B) pelvic magnetic resonance imaging showing lobulated subserosal myoma with internal hemorrhage and dilated pelvic vessels. (C) Specimen obtained from total laparoscopic hysterectomy and bilateral salpingo-oophorectomy.
2) Case 2 (stage II, patient #8)
A 49-year-old patient visited our clinic for new infiltration of a previously diagnosed myoma on abdomen pelvic CT (APCT). Transvaginal ultrasound showed a 7.3×4.6 cm myoma with extrinsic compression of both adnexa vessels (Fig. 3). On pelvic MRI, a 9.5 cm myoma with IVL along the IVC up to level 3 lumbar vertebrae was found. PET-CT showed mild fludeoxyglucose uptake across the entire uterus without uptake in IVC thrombus. The patient underwent TAH, BSO, and IVC mass removal followed by angioplasty. The final pathology report showed IVL of the uterine corpus and IVC. No pathologic abnormality was found on either ovaries or fallopian tubes. After complete resection, no recurrence was found after 6 months follow up, and the patient is still under surveillance.
An example of a stage II, 49-year-old patient with new infiltration of a previously diagnosed myoma on abdomen pelvic computed tomography. (A) Transvaginal ultrasound showing a myoma with extrinsic compression of both adnexa vessels and (B) the pelvic magnetic resonance imaging showing a 9.5 cm myoma with inferior vena cava involvement up to level 3 lumbar vertebra. (C) Specimen obtained from total laparoscopic hysterectomy and bilateral salpingo-oophorectomy, and inferior vena cava mass removal.
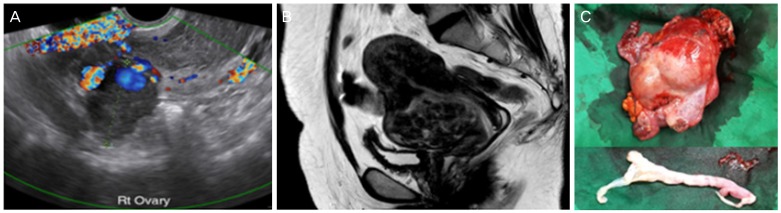
3) Case 3 (stage III, patient #9)
A 43-year-old patient visited the emergency department for syncope; she was on intravenous heparinization for a known intra-cardiac mass. Transvaginal sonography revealed a 4.5 cm pedunculated mass within the endometrium, 1 to 2 cm-sized multiple intramural myomas, and a 4.5 cm ill-defined mass around the iliac vessel with suspected retroperitoneal penetration (Fig. 4). APCT revealed a tortuous tubular mass within the endometrium with extension to the myometrium and through the bilateral pelvic vein to the left gonadal, renal vein, and IVC. Transthoracic echocardiography (TTE) showed an intracardiac mass in the right atrium with dynamic movement with cardiac cycle into right ventricle past the tricuspid valve. The patient underwent multidisciplinary surgery with a general surgeon and a cardiothoracic surgeon. A TAH with left salpingo-oophorectomy, intravenous mass removal through the dissection of the IVC, of both renal veins, the left gonadal and the internal iliac veins, in addition to removal of an intracardiac mass with extension to proximal pulmonary artery were performed under a 2-stage operation with complete cardiopulmonary bypass. The final pathology report indicated multiple submucosal leiomyomas, a hemorrhagic corpus luteal cyst of left ovary, and IVL on the uterine adnexa and the left broad ligament. Tissue samples from extrauterine lesions were consistent with IVL. After surgery, no remnant intracardiac mass was detected on follow up TTE, and an initial finding of mild pulmonary hypertension prior to the surgical procedure was normalized. However, on the 1-year follow up using transvaginal sonography, a 6.6 cm hypoechoic mass with a 2.6 cm internal cystic portion was detected on the right adnexa. APCT showed a 4.6 cm low attenuating mass in the right iliac fossa. The patient underwent right salpingo-oophorectomy (RSO), para-ovarian mass excision, and lymph node sampling. Longitudinal opening of the ovarian vessel exposed a rubbery, jelly-like material. The patient did not receive any adjuvant therapy and was free from disease recurrence on APCT after 6 years of follow up.

An example of a stage III, 43-year-old patient presenting with recurrent syncope episode. (A) magnetic resonance imaging showing a 7 cm-sized ‘comma’ shaped thrombosis, extending from the inferior vena cava intrahepatic portion to the right atrium. (B) The transthoracic echocardiography showing an intracardiac mass with dynamic movement past the tricuspid valve into the right ventricle. (C) Specimen from total abdominal hysterectomy, left salpingo-oophorectomy, and inferior vena cava and intracardiac mass removal. (D) One-year follow up showing localized recurrence at right iliac fossa found on abdomen pelvic computed tomography. (E) Specimen obtained from right salpingo-oophorectomy and para-ovarian mass excision.
4) Case 4 (stage IV, patient #12)
A 47-year-old patient visited our hospital for heavy menstrual bleeding and had a history of recurrent myoma. The patient underwent previous treatment with a gonadotropin-releasing hormone (GnRH) agonist for a 10 cm-sized myoma and had undergone laparoscopic myomectomy 2 years prior to visiting our hospital. On initial evaluation, transvaginal ultrasound showed the uterus enlarged to a 20-week gestational size and multiple intramural myomas (11.9 cm on the upper segment and 7.3 cm on the lower segment) with degeneration and internal necrotic lesion with the absence of increased regional blood flow (Fig. 5). The patient underwent total laparoscopic hysterectomy, RSO, left salpingectomy, and mass excision of multiple parasite myomas. Intraoperatively, myomas were observed on the uterine wall, the large bowel, and the omentum. The final pathology report indicated multiple leiomyomas with hydropic degeneration in the myometrium and omentum. After an uneventful one-month follow up, the patient was lost on the 6-month follow up. After 3 years, the patient presented at the emergency department complaining of lower abdominal pain and right back pain. Pelvic MRI showed a 12-cm mass on the right side of the pelvic cavity and a small nodule in both basal lungs. The differential diagnosis included a recurrent myoma with benign metastasizing leiomyomatosis and sarcoma with lung metastasis. On the second operation, a 10×8.0 cm pelvic mass, a 1.0×1.0 cm mass on the left infundibulopelvic ligament, and a 0.5×0.5 cm mass on the bladder serosa were completely excised. The final pathology report indicated leiomyoma with extensive hydropic degeneration. After one month, the patient underwent a separate video-assisted thoracoscopic surgery operation for wedge resection for a total of 8 pulmonary lesions. The final pathology report confirmed a BML with the largest dimension being 1.9 cm. On specific staining, the sample was focal positive for ER, PR, and SMA. On 3 months follow up, the patient had no evidence of recurrence on APCT, and the abnormal chest X-ray finding had resolved.
An example of a stage IV, 47-year-old patient presenting with heavy menstrual bleeding and history of previous myomectomy. After 3 years of primary surgery total abdominal hysterectomy, bilateral salpingo-oophorectomy, (A) the abdomen pelvic computed tomography showed recurrence with a 12 cm-sized pelvic mass and (B) bilateral lung nodules on chest computed tomography. Specimen obtained from (C) pelvic mass excision and (D) video-assisted thoracoscopic surgery guided resection of bilateral basal lung nodule.
Discussion
For the first time to our knowledge, we present a sizable case series from a single center in Korea. Analysis of clinical characteristics showed that these patients were mostly pre- or peri-menopausal and parous with a history of D&C procedures. Aside from patients with IVL extension to distant organs who presented with cardiac symptoms, most patients presented at the clinic because of symptoms similar to classical leiomyomas such as heavy menstrual bleeding, increase in myoma size, or lower abdominal discomfort. Tumor markers including CA125 and CA19-9 were not elevated beyond normal ranges. The results of the laboratory tests including those for creatinine, calcium, and phosphate were similar for early stage and late stage IVL. While a trend for high NLR in advanced stage IVL was observed, the standard deviation among sample values was too large for statistical significance. PLR was statistically higher in the late stage IVL group. A total of 2 stage II patients and one stage IV patient experienced recurrence on follow up.
As common as leiomyomas are, variants such as IVL and BML are considered extremely rare. Indeed, fewer than 200 cases of IVL have been reported after the first description by Birch-Hirschfeld in 1896. However, we gathered a sizable case series indicating that taking into consideration IVL and BML is important in differential diagnosis of aberrant leiomyoma, especially when a patient visits the clinic with a large myoma or increased size thereof, innumerable small myomas, or myomas with abnormal qualitative characteristics such as degeneration or internal necrosis. Although the etiology is currently unknown, recent molecular cytogenetic studies have suggested that IVL cases have a gene expression profile similar to that of uterine leiomyoma as well as leiomyosarcoma which explains their quasi-malignant behavior [11].
In order to stratify the clinical extent of IVL, we have adopted the concept of IVL staging proposed by Ma et al. [10]. Patients with stage I IVL are difficult to distinguish from classical leiomyoma based on routine blood tests and transvaginal sonography alone. Based on the size of the largest myoma on ultrasound, the size and number of myomas in stage I IVL are not consistent. A total 2 of 4 patients presented with a myoma of less than 5 cm and visited our hospital for abnormal uterine bleeding; thus, IVL was incidentally found on post-operative pathology. The 2 other patients with stage I IVL had huge myomas of 18 cm (patient #1) and 10 cm (patient #3) in size, which was in fact larger than the largest myoma of all other patients categorized in late stage IVL. The average size of the largest myoma in stage II IVL patients was 8.6 cm and that of stage III and IV IVL patients combined was 8.0 cm. In other words, stage I IVL patients were either incidentally diagnosed or likely would not have been missed due to the huge pelvic mass. Furthermore, no case of recurrence was observed in stage I IVL.
On the other end of the spectrum, patients with stage III or IV IVL would have been identified, given their cardiac symptoms or abnormal findings on chest X-ray. In our study, all stage III IVL patients had all distant lesions completely resected. Nonetheless, the importance of a multidisciplinary approach during the surgical procedure, including general surgeons and cardiothoracic surgeons cannot be more emphasized, as previous studies report on the challenges associated with complete resection of advanced stage IVL [12]. In the middle ground, the stage II IVL patients could have been easily missed on transvaginal ultrasound; APCT and pelvic MRI were the most useful diagnostic modality in our study. In terms of laboratory studies, subgroup analysis showed that NRL and PLR were higher in stage II IVL compared to stage I IVL. NLR was 14.6 vs. 1.51 and PLR was 0.25 vs. 0.13 for stage II IVL and stage I IVL, respectively. Recently, NLR and PLR have been suggested as markers for systemic inflammation in various solid tumors and non-cancerous conditions including endometriosis. In endometrial cancer, pre-operative NLR and PLR levels were associated with advanced stage, lymph node metastasis, and adverse clinical outcome including survival [13]. Similar to malignant conditions, systemic inflammation such as relative thrombocytosis, neutrophilia, and lymphocytopenia may underlie the acute phase of intravenous mass extension in stage II IVL. Overall, these patients in stage II IVL represent the cohort who will benefit the most from heightened suspicion by individual clinicians, because the recurrence rate in stage II IVL was found to be at least as high as stage III and IV IVL. The overall recurrence rate of 25.0% in our study is comparable to the previously reported rate, which ranged from 16.6% to 31.0% [1415].
Although IVL and BML were once thought of as distinct entities, evidence is accumulating on the shared origin of these leiomyoma variants with extrauterine manifestation [1617]. It is possible that cases with concurrent IVL and BML have been under-reported. Nonetheless, we have also performed a separate statistical analysis with the IVL group only to show that the trend and pattern of statistical significant is consistent either with or without the inclusion of the BML group.
Limitations to our study include the retrospective study design and the small sample size. A prospective study with a larger sample size would have permitted a more sophisticated statistical analysis regarding prognosis and treatment. Since the majority of IVL and BML patients are known to be pre-menopausal, identification of factors associated with disease recurrence may help clinicians make decisions regarding surgical castration. Young patients subjected to ovary-sparing procedures, especially for those who had stained positive for ER or PR markers, may have benefited from adjuvant therapy using GnRH agonist. The choice of adjuvant therapy was not consistent in our patient group.
IVL and BML are benign myoma variants with a paradoxically metastatic clinical presentation. Careful inquiry of systemic symptoms, the presence of underlying systemic inflammation, and a high index of suspicion are required for an optimal preoperative diagnosis. Furthermore, a multidisciplinary approach is necessary to improve outcomes from surgical resections.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.