Angiomyofibroblastoma of the vulva
Article information
Abstract
Angiomyofibroblastoma (AMFB) is an uncommon benign mesenchymal tumor. AMFB occurs almost in the vulvo-vaginal area of women. The gross features of AMFB are well-circumscribed so it clinically is often thought as Bartholin gland cyst or aggressive angiomyxoma. Usually, most tumors grow slowly, and patients do not feel pain. It also has low tendency for local recurrence. The histologic findings of the tumors are abundant thin-walled blood vessels with hypocellular and hypercellular areas. Almost all tumor cells have immunoreactivity for both desmin and vimentin. It also has estrogen and/or progesterone receptors, but staining for cytokeratin is negative. Here is a case of AMFB of the vulva occurring in a 40-year-old woman, involving the right labia majora. The patient described that her vulva mass grew in about few months. The maximum dimension of the tumor was measured as 2 cm, and we resected the tumor one month after as her second visit.
Introduction
Angiomyofibroblastoma (AMFB) is an unusual benign mesenchymal tumor. AMFB occurs primarily in the vulvo-vaginal area of middle-aged women [1-3]. The histologic findings of the tumors are abundant thin-walled blood vessels with hypocellular and hypercellular areas [4]. One of the differential diagnoses of AMFBs is angiomyxoma by its circumscribed borders. It can also observed the plump stromal cells and perivascular condensation in the stromal cells [5]. Almost all tumor cells have immunoreactivity for both desmin and vimentin, which also has estrogen and/or progesterone receptors; however, staining for cytokeratin showed to be negative [6]. Sometimes, AMFB is misdiagnosed as a Bartholin gland cyst due to its slow growing nature and possible formation of a pedunculated mass [7]. Here is a case of AMFB of the vulva occurring in a 40-year-old woman, involving the right labia majora.
Case Report
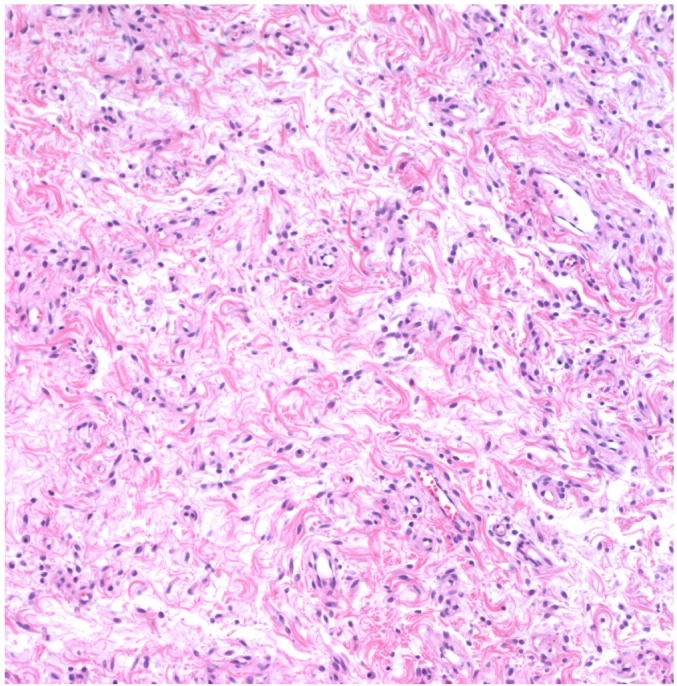
A 40-year-old woman came to our outpatient clinic with a painless vulvar mass that started few months before, which had gradually grown. At first, she ignored the mass, because it did not have any symptoms, despite its enlargement. However, she decided that she had to go the hospital because the size of mass enlarged and she feel uncomfortable. She did not had any previous gynecological surgery and her laboratory data (complete blood cell count, creatinine, coagulation, selology) showed no significant abnormalities. Physical examination showed a hardened mass of about 2 cm in diameter of the right labia majora with tense elastic consistency. On pelvic examination, the uterus and bilateral ovary showed no abnormalities and pelvic lymph nodes were not swollen. First, the clinical impression of the mass was bartholin cyst or lipoma. Therefore, we decided that simple tumor excision was the proper treatment for the mass, and it was subsequently performed one month after as her second visit. On gross examination, the mass was well circumscribed and had a soft to firm legion with a size of about 2×2 cm; no more grown compare to one month ago as her first visit. The color of the mass cut surface was light gray to tan homogeneously. Surgical margins of the lesion were clear. Microscopically, the tumor demonstrated admixture of hypocelluar and hypercellular area in the background of edematous stroma. The abundant vessels of various wall thickness were distributed in the collagenous stroma. The stroma consisted of spindle and ovoid stromal cells with eosinophilic cytoplasm and no mitotic features or significant nuclear atypia (Fig. 1). The tumor also has estrogen and/or progesterone receptors and has immunoreactivity for vimentin (Fig. 2).
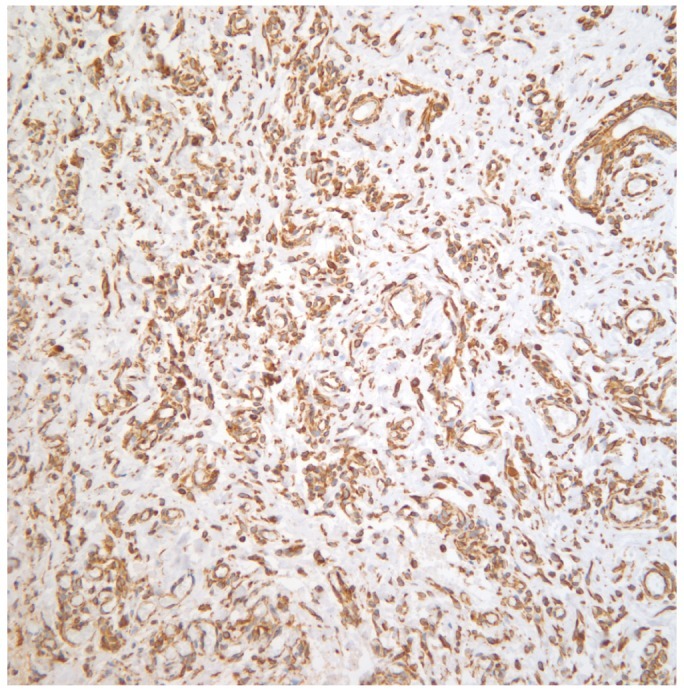
Spindles cells around blood vessels without bland nuclei in the background of dense collagenous matrix (vimentin, ×100).
Currently, the patient was follow up was lost for about 7 years and we decided to follow up with her by a telephone call. She said she almost forgot about the mass removal event and there is no evidence of recurrence.
Discussion
AMFB was became generally known by Fletcher et al. [8] in 1992, who described ten cases involving the vulva AMFB occurs primarily in the vulvo-vaginal area (predominantly the vulva) of middle-aged women. Rare cases have also been reported to arise in the scrotum and the inguinal area in males [8,9]. Between 1999 and 2013, there were only 57 publications in english literature of AMFB. With biologic behavior, all published reports suggest a benign clinical outcome in patients with AMFB. To our knowledge, only one reported case underwent a sarcomatous transformation [10] and no recurrence. The occurring average age of female is 45.8 years and rather slow growing (from few weeks to 13 years) without pain [5]. Clinically, these tumors are misdiagnosed as Bartholin gland cyst, inguinal hernia, leiomyoma, or mesenchymal tumors, such as lipoma and liposarcoma [11]. On gross examination of the tumor, they are typically well circumscribed and hard with rubbery consistency, with size that ranged from 0.5 to 12 cm. Most of the tumors are pink in color [5]. Microscopic examination shows well-demarcated lesion and alternating hypercellular and hypocellular edematous legions with abundant blood vessels. Nuclear atypicality or mitotic figures are rare and the tumor cells tend to cluster around blood vessels [5]. Sometimes adipocytes are scattered within the mass, and these tumors have been classified as the "lipomatous" variant of AMFB. AMFB can be distinguished from the aggressive angiomyxoma by its circumscribed borders; AMFB has chubby stromal cells and the stromal cell condenses the perivascular area [12]. Immunohistochemical findings show that the tumors are staining for vimentin and desmin in most cases. The tumor cells also show variable expression for muscle actin and are positive for estrogen and/or progesterone receptors [5]. Because of this hormonal receptor expression, the tumor suggests that it might arise from hormonally responsible mesenchymal cells [3]. The patient underwent simple excision with clear margin of the lesion. Despite our recommendation for regular follow up, the patient did not comply for seven years and we finally decided to follow up with her by a telephone call. She said she almost forgot about the mass removal event and there is no evidence of recurrence. This paper aims to announce AMFB of vulvar as an rare tumor. The treatment of choice is a surgical excision with clear margins.
Notes
No potential conflict of interest relevant to this article was reported.