Efficacy of luteal estrogen administration and an early follicular Gonadotropin-releasing hormone antagonist priming protocol in poor responders undergoing in vitro fertilization
Article information
Abstract
Objectives
We investigated whether luteal estrogen administration and an early follicular Gonadotropin-releasing hormone antagonist (E/G-ant) priming protocol improves clinical outcomes in poor responders to controlled ovarian stimulation for in vitro fertilization (IVF)-embryo transfer, and identified underlying mechanisms.
Methods
This restrospective study consisted of 65 poor responders who underwent the E/G-ant priming protocol. Sixty-four other poor responders undergoing conventional protocols without pretreatment were included as the control group. Clinical outcomes were compared between 2 groups.
Results
The E/G-ant priming protocol group exhibited improvements over the control group in terms of the number of retrieved oocytes (3.58±2.24 vs. 1.70±1.45; P=0.000), mature oocytes (2.68±2.11 vs. 1.65±1.23; P=0.000), fertilized oocytes (2.25±1.74 vs. 1.32±1.26; P=0.001), good embryos (1.62±0.91 vs. 1.14±0.90, P=0.021). Day 3 follicle-stimulating hormone (FSH; 8.40±4.84 vs. 16.39±13.56; P=0.000) and pre-ovulation progesterone levels (0.67 vs. 1.28 ng/mL; P=0.016) were significantly higher in the control group than in the E/G-ant priming group. The overall rate of positive human chorionic gonadotropin tests was higher in the E/G-ant priming group than in the control group (32.3% vs.16.1%; P=0.039). Also, clinical pregnancy rate (26.2% vs. 12.5%; P=0.048) and the rate of live births (23.1% vs. 7.1%; P=0.023) were significantly higher in the E/G-ant priming group than in the control group.
Conclusion
The E/G-ant priming protocol would lead to promising results in poor responders to IVF by suppressing endogenous FSH and by preventing premature luteinization.
Introduction
Controlled ovarian stimulation (COS) is a key determinant of the success of in vitro fertilization (IVF)-embryo transfer (ET). Extensive research has established many combinations of medications and COS protocols for IVF-ET. Nevertheless, there are always patients who respond poorly to COS protocols for various reasons, including reduced ovarian reserves and hormonal imbalances [12]. The prevalence of poor ovarian response (POR) can vary from 5.6% to 35.1% — depending on how the term is defined — and is gradually increasing among IVF patients [345678]. Numerous studies and modified protocols have been proposed over the past 20 years for poorly responding patients. It is frustrating to note, however, that there has been no efficient treatment ensuring notable improvement of ovarian response in patients [791011]. Women who respond poorly to various COS methods generally have lower numbers of retrieved oocytes and transferable embryos, and inevitably have lower clinical pregnancy rates than those of normal responders [81213].
In a COS cycle, follicles are expected to grow concurrently in response to exogenous gonadotropins in order to accomplish simultaneous maturation. Conversely, marked discrepancies in follicular size in the early follicular phase result in decreased oocyte maturation and fertilization potential, which negatively impact the number of transferable embryos and the probability of conception [141516]. This heterogeneity of follicular growth in COS cycles has been observed more frequently in POR [3141718]. Although the physiological mechanism implicated in this process remains poorly understood, a few hypotheses have focused on premature dominant follicle selection after the rise of follicle-stimulating hormone (FSH) in the late luteal phase, or on different developmental levels of each recruited follicle [1819]. To reduce heterogeneity of follicles, estrogen pretreatment in late luteal phases in COS cycles were proposed, but estrogen pretreatment did not lead to satisfying results in clinical pregnancy rates, regardless of improvement to follicular size homogeneity and increased numbers of retrieved oocytes [172021222324]. In addition, some authors postulated that applying a Gonadotropin-releasing hormone (GnRH) antagonist in the follicular phase before ovarian stimulation could create an opportunity to lengthen the recruitment phase of the cycle, thereby allowing the rescue of more follicles by suppressing endogenous FSH and preventing corpus luteum formation without compromising the ovarian stimulatory response of poor responders [25262728].
Cakmak et al. [3] suggested a protocol that focused on the heterogeneity of antral follicle responsiveness to gonadotropins during the early follicular phase. In order to synchronize the growth of a pool of follicles they applied estrogen priming during the late luteal phase and following pretreatment with the GnRH antagonist for 7 days of the early follicular phase prior to gonadotropin stimulation. The authors reported improved ovarian responsiveness during COS, although they could not describe clinical pregnancy rates between protocols due to the study design [3]. Furthermore, the duration of GnRH antagonist pretreatment was relatively longer than other GnRH antagonist pretreatment protocols [25262728], so that total duration of the IVF-ET cycle was relatively prolonged. Although the mechanism was not made clear, prolonged duration of treatment might be implicated as a cause of premature luteinization (PL) in COS [2930]. PL is understood to be a subtle increase in serum progesterone levels observed during the late follicular phase in COS, which reflects only the total amount of progesterone secreted by maturing follicles in the absence of any premature uncontrolled luteinizing hormone (LH) surge [31]. PL has been observed frequently in elderly or poorly responding patients [323334], and in addition, recent meta-analyses have found that PL had more adverse effects on IVF outcomes in poor responders than in normal or high responders [353637]. In line with these trials, we conducted 7–10 days of luteal estrogen administration, followed by 5 consecutive days of early follicular GnRH antagonist (E/G-ant) priming protocol for POR (Fig. 1).
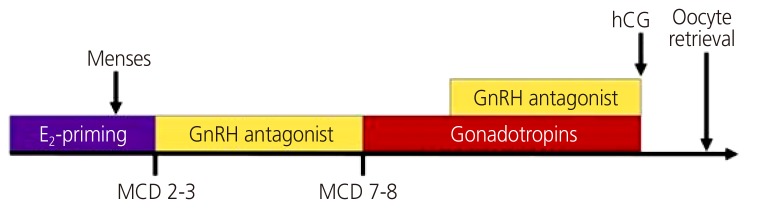
Diagram of the early follicular Gonadotropin-releasing hormone (GnRH) antagonist (E/G-ant) priming protocol.
E2, estradiol; MCD, menstrual cycle days; hCG, human chorionic gonadotropin.
The primary aim of this study was to investigate whether the luteal estradiol (E2) and E/G-ant priming protocol protocol would improve ovarian responses and clinical outcomes in poor responders, and to identify the mechanisms underlying favorable outcomes in poor responders, particularly with respect to changes in hormonal status.
Materials and methods
1. Patient selection
This retrospective, single-center cohort study was conducted at the Infertility Center at Cheil Hospital in Seoul between May 2014 and July 2016. We enrolled 65 consecutive patients who met the Bologna criteria [38]. The Bologna criteria states that POR is defined by at least 2 of the following 3 features that must be present: 1) advanced maternal age (≥40 years) or any other risk factor for POR; 2) previous POR (≤3 oocytes with a conventional stimulation protocol); and 3) an abnormal ovarian reserve test (i.e., antral follicle count, 5–7 follicles or anti-mullerian hormone [AMH], 0.5–1.1 ng/mL) [38]. Sixty-four other women categorized into POR according to the Bologna criteria were selected as controls and underwent a conventional GnRH antagonist protocol during the study period. All patients had been previously diagnosed with female infertility based on an infertility evaluation that included serum basal hormone levels (E2, FSH, LH, thyroid-stimulating hormone [TSH], and prolactin levels on menstrual cycle days [MCD] 2 or 3), as well as a hysterosalpingogram and hysteroscopy or laparoscopy as needed. All patients had normal menstrual cycles with a range of 24–35 days, normal serum TSH and prolactin levels and had no other factors of infertility except for POR. Among 64 patients in the control group, 8 patients were excluded because of high E2 levels or abnormal ultrasound findings on the second or third MCD. Institutional Review Board has been exempted due to retrospective nature of the study.
2. Luteal E2 administration and E/G-ant priming protocol
Patients were put on 4 mg of daily oral E2 valerate (Progynova; Bayer Healthcare Pharmaceuticals, Wayne, NJ, USA) for an estrogen priming cycle beginning a week following their previous ovulation until menses. On MCD 2 or 3, patients visited the center for measurement of baseline FSH, LH, and E2 levels, ultrasound examination for antral follicle counting, and endometrial thickness measurement. Next, the patients began 0.25-mg daily subcutaneous injections of GnRH antagonist (cetrorelix acetate) (Merck KGaA, Darmstadt, Germany) on MCD 2 or 3. After 5 days of GnRH antagonist pretreatment, patients started on 375–450 IU of human menopausal gonadotropin (hMG) (Menopur; Ferring Pharmaceuticals, Tarrytown, NY, USA) at the mid-follicular phase of the cycle (MCD 7–8). The GnRH antagonist was added for the second time when the largest follicle measured >12 mm in order to prevent premature ovulation before the human chorionic gonadotropin (hCG) trigger. hCG was administered when the leading follicle measured >18 mm and the remaining follicles were >10 mm.
3. Conventional GnRH antagonist protocol (control group)
The conventional GnRH antagonist protocol in the control group did not apply hormonal pretreatment during the luteal period and subsequent early follicular phase. On MCD 2 or 3, patients visited the center for measurement of their baseline FSH, LH, and E2 levels, for antral follicle counting via ultrasound examination, and for measurement of endometrial thickness. For the conventional antagonist protocol, patients were administered 375–450 IU of hMG (Menopur; Ferring Pharmaceuticals) via daily subcutaneous injection beginning on MCD 3 for ovarian stimulation. The GnRH antagonist was added when the largest follicle measured >12 mm in order to prevent premature ovulation before the hCG trigger. Recombinant hCG (Ovidrel; Merck Serono, Geneva, Switzerland) was administered when the leading follicle measured >18 mm and the remaining follicles were >10 mm.
4. Oocyte retrieval, embryo culture, and transfer procedure
Oocytes were harvested via transvaginal ultrasound-guided follicular puncture 35–36 hours after hCG administration. Metaphase oocytes were fertilized by an intracytoplasmic sperm injection (ICSI) technique 4–6 hours after oocyte retrieval. Embryos were cultured separately and scored according to the modified Gardner and Schoolcraft grading system [39]. The number of embryos transferred was based on the number of good embryos (above grade II) together with the circumstances of the patient. Embryos were transferred on either post-fertilization day 2 or 3 under abdominal ultrasound guidance.
5. Outcome measures related to IVF and pregnancy outcomes
In order to analyze the effectiveness of the E/G-ant priming protocol, we compared the IVF-ET outcome, hormonal status and pregnancy outcome with those of the control group. IVF-ET outcomes included the number of mature (metaphase II [MII]) oocytes, total number of oocytes retrieved, oocyte maturity rate (MII oocyte number/total oocyte number), fertilization rate (percentage of 2PN stage zygotes approximately 16 hours after ICSI treatment) and the number of good embryos (above grade II according to the graduated embryo score [GES] grading system). To analyze serial hormonal status, changes of serum E2 and P4 levels were compared between E/G-ant priming protocol group and the control group on MCD 3, the GnRH antagonist starting day when the largest follicle measured >12 mm, and the day of hCG injection. Serum beta hCG levels were measured 12 days after ovum pick-up, and values above 5.0 IU were considered positive. Clinical pregnancy was defined as the presence of an intrauterine gestational sac with a yolk sac, a fetal pole, and fetal heart pulsations. The live birth rate was defined as delivery of a viable baby after 24 weeks of gestation.
6. Statistical analysis
Data are statistically presented in terms of the mean±standard deviation, number of cases, and percentage when appropriate. We used Student's t-tests to evaluate continuous parameters. Chi-squared tests and Fisher's exact tests, as appropriate, were used to compare clinical pregnancy rates. A P-value <0.05 was considered statistically significant. The statistical analysis was performed with SPSS ver. 22.0 (IBM Co., Armonk, NY, USA).
Results
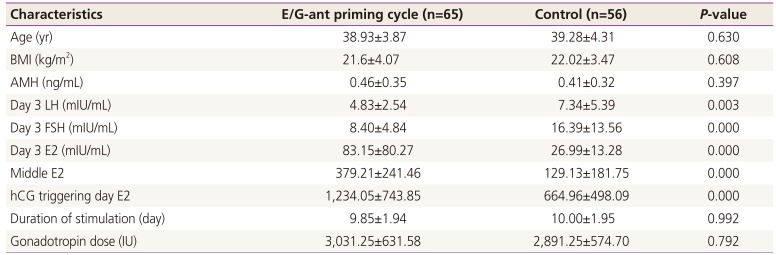
Among the 64 patients enrolled in the control group, 8 patients were excluded because of abnormal baseline hormonal levels or ultrasound findings on MCD 2 or 3, while no one was excluded from the E/G-ant priming group. The E/G-ant priming group and the control group were generally well matched in terms of baseline characteristics known to affect clinical pregnancy rates, such as age, previous pregnancy, body mass index and AMH levels (Table 1). The 2 groups did not differ significantly in the total dose of gonadotropin for stimulation or the duration of stimulation (Table 1). However, the levels of E2 (E/G-ant priming group vs. control group; 83.15±80.27 vs. 26.99±13.28; P<0.001) and FSH (E/G-ant priming group vs. control group; 8.40±4.84 vs. 16.39±13.56; P<0.001) in samples taken at the beginning of the cycle differed significantly between groups. Also, E2 level sampled on the day of hCG triggering was higher in the E/G-ant priming group than in the control group (E/G-ant priming group vs. control group; 1,234.05±743.85 vs. 664.96±498.09; P<0.001; Table 1).

Comparison of the clinical characteristics of early follicular Gonadotropin-releasing hormone antagonist priming cycle and control groups
Serum progesterone levels were initially documented in 52 patients from the E/G-ant priming group and 45 patients in the control group on MCD 2 or 3. As shown in Fig. 2, group progesterone levels did not differ at the beginning of the cycle (E/G-ant priming group vs. control group; 0.26±0.17 vs. 0.40±0.25 ng/mL; P=0.156) or on the mid-follicular antagonist administration day (E/G-ant priming group vs. control group; 0.27±0.24 vs. 0.41±0.20 ng/mL; P=0.066). However, serum progesterone levels were significantly higher in the control group than in the E/G-ant priming group before ovulation (E/G-ant priming group vs. control group; 0.67±0.53 vs. 1.28±1.12 ng/mL; P=0.016).
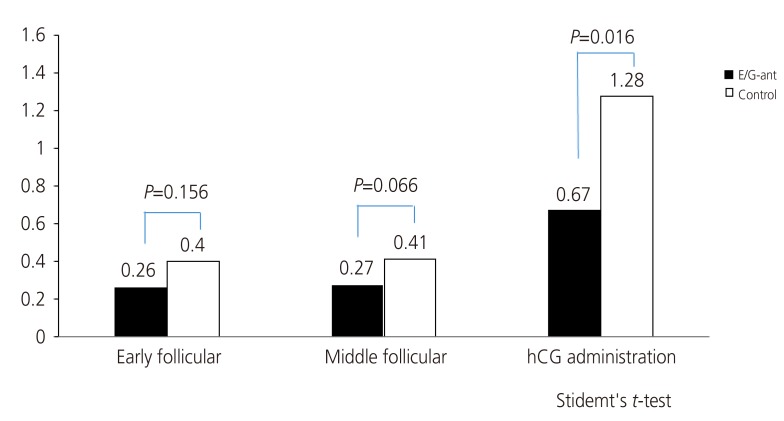
Serum progesterone level during controlled ovarian stimulation.
E/G-ant, early follicular Gonadotropin-releasing hormone antagonist.
Clinical outcomes in each group are shown in Table 2. The overall success rate of yielding at least one oocyte after the procedure of ovum pick up in the E/G-ant priming group (90.8% [59/65]) was greater than that in the control group (80.4% [45/56]), although this lacked statistical significance. However, the number of oocytes retrieved (3.58±2.24 vs. 1.70±1.45; P=0.000) and the number of mature oocytes (2.68±2.11 vs. 1.65±1.23; P=0.000) were significantly greater in the E/G-ant priming group. The number of successfully fertilized embryos (2.26±1.62 vs. 1.52±0.72; P=0.012) and good embryos according to the GES grading system (1.62±0.91 vs. 1.14±0.90; P=0.021) was also greater in the E/G-ant priming group than in the control group (Table 2).

Clinical outcomes of early follicular Gonadotropin-releasing hormone antagonist priming and control groups
The overall rate of positive hCG tests was higher in the E/G-ant priming group than in the control group (32.3% [21/65] vs.16.1% [9/56]; P=0.039). Also, clinical pregnancy rate for overall study group (26.2% [17/65] vs. 12.5% [7/56]; P=0.048) and the rate of live births (23.1% [15/65] vs. 7.1% [4/56]; P=0.023) were significantly higher in the E/G-ant priming group than in the control group.
Discussion
POR to COS is a serious problem due to a quantitative reduction in the follicular response and a consequent decrease in the retrieved oocyte number, transferable embryo number and pregnancy rate in comparison to normal responders [81340414243]. Therefore, it is essential to identify an optimal stimulation protocol to maximize the quality and number of retrieved oocytes so that designated poor responders can achieve pregnancy.
In a COS cycle, exogenous gonadotropins are administered in order to achieve simultaneous maturation of follicles. Some authors have postulated that FSH elevation during the luteal-follicular transition might cause asynchronous follicular size and, ultimately, may reduce the follicular cohort available for recruitment [172344]. Although the physiological mechanisms implicated in this process remain poorly understood, a few strategies have been proposed in order to suppress this phenomenon in POR [31720212223252627]. Taking into account all these considerations, we hypothesized that using estrogen administration in the late luteal phase of the preceding menstrual cycle followed by GnRH antagonist pretreatment in the beginning of the follicular phase could be a promising method for suppressing endogenous FSH during the luteal-follicular transition and early follicular phase, and for promoting and synchronizing follicle development without impairing developmental competence of oocytes. In the present study, we modified the “delayed start” GnRH antagonist protocol in the work of Camak et al. [3] by shortening GnRH antagonist pretreatment to 5 days in the beginning of the follicular phase for in order to optimize patient hormonal status in COS cycles, as well as to minimize costs and maximize patient convenience. The purpose of this retrospective cohort study was to evaluate the impact of luteal estrogen administration and a 5-day course of E/G-ant priming protocol in poor responders. Secondly, we sought to understand the mechanisms that bring favorable outcomes, particularly with regard to changes in hormonal status.
Our study findings are consistent with previous studies that demonstrate greater numbers of retrieved oocytes and transferable embryos by using luteal estrogen or GnRH antagonist pretreatment in comparison to controls [317202123242526]. With respect to hormonal status, basal FSH levels in the E/G-ant protocol group were notably lower than basal FSH levels in the control group. Conversely, E2 levels in the E/G-ant protocol group were significantly higher than the E2 levels of patients in the control group. In our opinion, these results indicate that FSH elevation was sufficiently suppressed before the start of the follicular phase, and therefore, the E/G-ant priming protocol might effectively inhibit premature dominant follicle selection.
The association of clinical outcomes of COS cycles with PL remains controversial. Many studies have suggested that PL adversely affects IVF-ET cycle outcomes [32454647], whereas other authors have reported that this condition does not have any negative effects on the outcomes of COS cycles [48495051]. While clinical observations have had mixed results, several possible mechanisms have been proposed to explain the pre-ovulatory progesterone rise that has been observed among IVF patients. In some findings, the level of pre-ovulatory progesterone was positively related to the number and size of multiple follicles, the amount of exogenous gonadotropin, and the number of oocytes retrieved. Therefore, it was concluded that PL is usually observed in patients displaying a good response to ovarian stimulation [29515253]. In contrast, several papers have reported that PL is more prevalent in older or poorly responding patients despite relatively small number of oocytes [323334]. Furthermore, recent meta-analysis studies have found that PL had a more detrimental effect on the probability of pregnancy achievement in poor responders than in good responders in IVF-Et cycles [353637]. Although the mechanism was not clear, this could be explained by the fact that poor responders need longer periods of stimulation, and thus a significantly higher total FSH dosage than good responders [2930]. Also, Younis et al. [34] tried to explain this phenomenon in the context of POR with concepts of increased LH sensitivity. Additionally, PL may influence the endometrium, leading to impaired endometrial receptivity, which has negative effects on clinical pregnancy rates [3654]. In a recent study suggested that elevated pre-ovulatory progesterone level due to increased progesterone production per follicle (high PFI) was detrimental to IVF outcomes, but not if it is a consequence of additional follicular recruitment [55]. In our study, although the E2 levels of patients in the E/G-ant priming group on hCG triggering day and the number of retrieved oocytes exceeded these values in the control group, P4 levels remained significantly low in the E/G-ant priming group. Also, the E/G-ant priming group showed improved pregnancy outcomes compared to the control group in our study. These data indicate that the E/G-ant priming protocol effectively inhibits PL such that it may have positive effects on clinical pregnancy outcomes.
According to a recent meta-analysis, the clinical pregnancy rate of poor responders in an IVF-ET cycle averages 14.8%, whereas normal patients have a 34.5% pregnancy rate [56]. In our study, the overall rate for positive hCG tests in the E/G-ant priming protocol was 32.3%, and the rate of live births was 23.1%. To the best of our knowledge, these improved clinical pregnancy rates have not yet been reported in earlier studies of POR.
In conclusion, for patients with poor ovarian reserve who plan to undergo IVF, poor quality and a low quantity of oocytes have been major limitations on standard IVF-ET cycles. This luteal E2 administration and E/G-ant priming protocol would yield more mature oocytes and transferable embryos and, consequently, better clinical pregnancy rates than conventional GnRH antagonist IVF protocols. Nevertheless, the total number of analyzed patients was small. Accordingly, further prospective and randomized clinical trials are warranted to verify the findings reported herein.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.