 |
 |
- Search
| Obstet Gynecol Sci > Volume 60(4); 2017 > Article |
Abstract
Fibroepithelial polyp (FEP) and lymphangioma circumscriptum (LC) of the vulva are rare diseases that occur generally in young to middle-aged women. The pathogenesis of FEP is not clearly understood. Several previous cases have suggested that a hormonal influence may be a predisposing condition for developing FEP with or without chronic inflammation. A 68-year-old postmenopausal woman presented with a history of multiple raised lesions on the vulva with a 1-year duration. Additionally, a pedunculated mass had appeared 6 months earlier in the left lower labia minora. The patient underwent simple excision by electrocautery. The final pathological diagnosis was FEP with LC. In this case, the development of FEP was associated only with chronic inflammation induced by LC. Therefore, the case supports the hypothesis that a chronic inflammatory process may be related to the development of FEP even without hormonal influence.
Fibroepithelial polyp (FEP) of the vulva is a very rare and benign disorder that occurs generally in young to middle-aged women [1]. Vulvar FEP appears to have a hormonal association, as patients may be pregnant at diagnosis or have a history of hormonal therapy [2]. Lymphangioma circumscriptum (LC) of the vulva is a very rare and benign disorder of the lymphatics located in the deep dermal and subcutaneous tissues. Vulvar LC is characterized by dilation of superficial dermal lymphatic channels, resulting in localized papules and vesicles.
The first case of vulvar FEP was described by Ostor et al. [3] in 1988. Since then, two additional cases have been reported, associated with other diseases (congenital lymphedema [4] and psoriasis [5]). However, there has not been a reported FEP case associated with LC. We present the first report of a case of vulvar FEP in a postmenopausal woman that is uniquely associated with vulvar LC.
A 68-year-old postmenopausal woman presented with a history of multiple raised lesions over the vulva with a 1-year duration. Furthermore, a pedunculated solid mass appeared 6 months after the lesions in the left lower labia minora. The patient was asymptomatic initially, but later experienced malodorous discharge and pruritis. She had a clinical history of radiation therapy due to early stage of rectal cancer at 30 years ago and lymphadenopathy of the left inguinal region more than 5 years ago.
On physical examination, there were multiple frog spawnlike lesions measuring about 10 cm×5 cm on both sides of the vulva with a malodorous discharge. A large (5 cm×3.5 cm) pedunculated polyp was observed in the left lower labia minora. This pedunculated polyp had an ulcerated surface and was firm-to-hard in consistency. There were several grouped papules of similar morphology over the left upper thigh (Fig. 1A). Laboratory evaluation including hematologic, urinary, and tumor markers were within normal limits. Physical examination and ultrasonography of pelvic organs revealed no abnormal findings. Subsequently, enhanced magnetic resonance imaging scans demonstrated a 3.8 cm×3.3 cm×2 cm, pedunculated, exophytic lesion with connection to the left vulva. The preoperative imaging diagnosis was a benign tumor, such as fibroma or leiomyoma. The patient underwent simple excision by electrocautery and a carbon dioxide (CO2) laser was used to vaporize the lesion superficially. The postoperative course was uneventful. Six months later, the patient visited the hospital for a postoperative check-up. A physical examination revealed the absence of any gynecological abnormality (Fig. 1B).
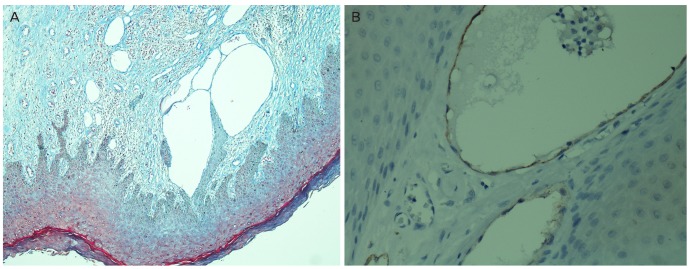
The lesions were composed of large pedunculated nodules and cluster of small polyps. The large nodules were well covered by hyperplastic epidermis and cored with edematous fibrous tissue with some inflammatory cells (Fig. 2A). The stromal cells were reactive for smooth muscle actin but not for S-100. The large nodules also exhibited focal dilated lymphatics near the papillary dermis. The small polyps exhibited typical LC in the papillary dermis, confirmed through immunostaining for lymphatic marker, D2-40 (Fig. 2B). The final pathological diagnosis was FEP with LC and the lesions were considered to be acquired lesions.
The report complies with the current laws of our country, and informed consent was obtained from the patients' who participated. The patient's information was enrolled in a paper approved by the Gumi CHA hospital institutional review board.
FEP is a rare, locally infiltrative but non-metastasizing tumor of pelvic soft tissue seen mostly in women of child-bearing age [1]. The most common clinical presentation of FEP is as a painless mass. Our patient had a 5-cm-sized pedunculated painless mass with a cluster of small polypoid LC lesions. Acquired LC of the vulva is also very rare [6]. The lesions typically appear approximately 7 to 15 years after lymph node dissection and therapy of the genitalia [7]. In the case, she had a history of low anterior resection for rectal cancer and underwent radiotherapy over 31 years ago. The most characteristic clinical presentation of vulvar LC is multiple small raised frog spawn-like lesions with watery discharge and sometimes coexistent lymphedema extending to the adjacent abdomen or thigh skin.
The normal treatment for FEP is surgical excision, but there is no standard management for vulvar LC. Consequently, excisional surgery and CO2 laser are the most commonly used treatment modalities. The CO2 laser therapy has been selected as an effective treatment for LC. This treatment is good for small, superficial lesions. In the present case, excision was performed by electrocautery while CO2 laser therapy was utilized for superficial LC lesions.
The pathogenesis of FEP of the vulva is not clearly understood. Some authors suggest a reactive hyperplastic process involving the distinctive subepithelial mesenchyma of the lower female genital tract [8]. Several previous cases suggested a hormonal influence with or without chronic inflammation as a predisposing condition for developing FEP. One previous case suggested hormonal changes induced by pregnancy as a predisposing factor for the development of FEP [9]. In addition, two cases demonstrated that hormonal influence with chronic inflammation is a predisposing factor for FEP. The first of those cases was a 16-year-old girl who developed FEP in association with congenital lymphedema; and the second was a 35-year-old woman with psoriasis who developed a 15 cm FEP localized in the left labium [4,5]. Histologically, the stromal cells of FEP have estrogen and progesterone receptors. Thus, hormonal influence may be a prerequisite condition for the development of FEP, as shown through an analysis of previous cases, clinical features, and histological findings. However, in the present case, the development of FEP was not associated with hormonal change. Instead, a chronic inflammation process induced by LC may have been the only predisposing factor. The patient was a postmenopausal woman who had not received hormonal therapy and had developed the LC lesion first, followed 6 months later by the FEP.
To the best our knowledge, this is the first reported case in the literature of FEP with LC. Furthermore, chronic inflammation induced by LC was the predisposing condition for the development of FEP. Hence, this case could support the hypothesis that a chronic inflammatory process is related to the development of FEP even without hormonal influence.
References
1. Nucci MR, Fletcher CD. Vulvovaginal soft tissue tumours: update and review. Histopathology 2000;36:97-108. PMID: 10672053.


2. McCluggage WG. A review and update of morphologically bland vulvovaginal mesenchymal lesions. Int J Gynecol Pathol 2005;24:26-38. PMID: 15626915.

3. Ostor AG, Fortune DW, Riley CB. Fibroepithelial polyps with atypical stromal cells (pseudosarcoma botryoides) of vulva and vagina: a report of 13 cases. Int J Gynecol Pathol 1988;7:351-360. PMID: 3229895.


4. Orosz Z, Lehoczky O, Szoke J, Pulay T. Recurrent giant fibroepithelial stromal polyp of the vulva associated with congenital lymphedema. Gynecol Oncol 2005;98:168-171. PMID: 15963814.


5. Dane C, Dane B, Cetin A, Erginbas M, Tatar Z. Association of psoriasis and vulval fibroepithelial polyp: first reported case. Am J Clin Dermatol 2008;9:333-335. PMID: 18717609.


6. Verma SB. Lymphangiectasias of the skin: victims of confusing nomenclature. Clin Exp Dermatol 2009;34:566-569. PMID: 19456771.


7. Okur MI, Kose R, Yildirim AM, Cobanoglu B. Lymphangiectasia of the vulva accompanying congenital lymphedema. Dermatol Online J 2009;15:13.
8. Nucci MR, Young RH, Fletcher CD. Cellular pseudosarcomatous fibroepithelial stromal polyps of the lower female genital tract: an underrecognized lesion often misdiagnosed as sarcoma. Am J Surg Pathol 2000;24:231-240. PMID: 10680891.


9. Zulfikaroglu E, Kilic S, Taflan S, Tarhan I, Akbay S, Mollamahmutoglu L. Vulvar fibroepithelial stromal polyp in the early pregnancy. Van Tip Dergisi 2013;20:88-90.
Fig. 1
Clinical appearance of the vulva. (A) Preoperation. Multiple frog spawn-like lesions and a large (5 cm×3.5 cm) pedunculated polyp were present. (B) Postoperation. The lesions were no longer present. M, fibroepithelial polyp.
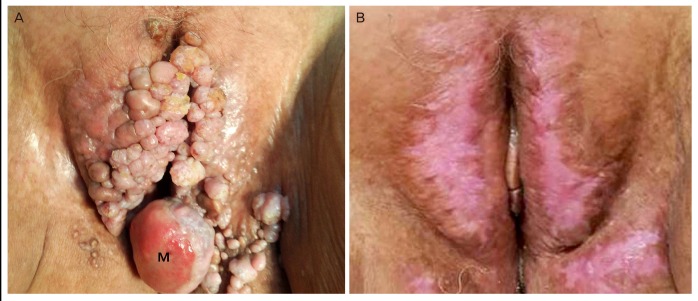
Fig. 2
Pathologic findings of lesions. (A) The large nodule revealed diffuse fibrous stroma and hyperplastic epidermis where few lymphatic vessels were dilated (trichrome stain, ×40). (B) The dilated lymphatic vessels were lined by endothelial cells positive for D2-40. Adjacent small blood vessels were unstained by D2-40 (immunostain for D2-40, ×200).
-
METRICS

- Related articles in Obstet Gynecol Sci
-
A case of giant fibroepithelial polyp of the vulva.2010 February;53(2)




















