 |
 |
- Search
| Obstet Gynecol Sci > Volume 60(4); 2017 > Article |
Abstract
Herlyn-Werner-Wunderlich syndrome is a rare congenital anomaly of the urogenital tract, which is characterized by the triad of uterus didelphys, obstructed hemivagina, and ipsilateral renal agenesis. It usually presents at puberty with pelvic pain, dysmenorrhea, and a vaginal or pelvic mass. Although rare, it may present with purulent vaginal discharge due to secondary infection of the obstructed hemivagina, making diagnosis difficult. A careful pelvic examination to identify the cervix and vagina is the key to the diagnosis of M├╝llerian duct anomalies and magnetic resonance imaging can provide additional useful information. The optimal treatment is full excision and marsupialization of the obstructing vaginal septum so that both uteri can drain through the patent vagina. The authors report a case of a 22-year-old female with an unusual presentation of Herlyn-Werner-Wunderlich syndrome complicated by pyocolpos, which was successfully managed by vaginal septum resection and drainage of pus.
Herlyn-Werner-Wunderlich syndrome (HWWS) is a rare congenital urogenital anomaly characterized by the combination of uterus didelphys with obstructed hemivagina and ipsilateral renal agenesis [1,2]. It is usually diagnosed after menarche, with a clinical presentation of dysmenorrhea, recurrent abdominal pain, irregular menses, and sometimes a palpable pelvic mass due to hematocolpos [1]. Rarely, patients may develop pyohematocolpos, pyosalpinx, and peritonitis as a result of an ascending infection due to retained discharge or menstrual blood in the obstructed hemivagina [3]. Symptoms vary depending on the uterovaginal relationship in individual cases, making diagnosis difficult. A careful pelvic examination to identify the cervix and vagina is the key to the diagnosis of M├╝llerian duct anomalies. A magnetic resonance imaging (MRI) can provide additional useful information. The optimal treatment is full excision and marsupialization of the obstructing vaginal septum so that both uteri can drain through the patent vagina [2]. We present an unusual case of a 22-year-old female with HWWS complicated by pyocolpos, which was successfully managed by vaginal septum resection and drainage of pus.
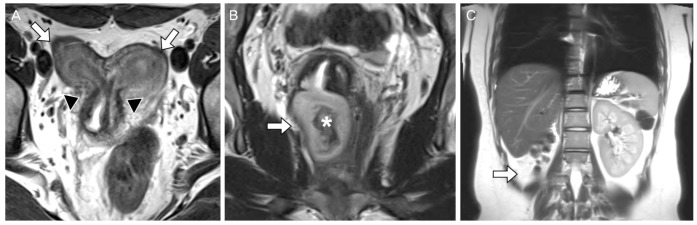
A 22-year-old women (gravida 0 and para 0) visited our gynecology department with the chief complaint of a foul-smelling vaginal discharge with intermenstrual bleeding. The patient denied fever, chills, nausea, vomiting, or diarrhea. Past medical and surgical history was unremarkable. Menarche had occurred at the age of 13 years. She still had some brownish discharge although her last menstrual period was 2 weeks ago. She had no complaints of dysmenorrhea, dyspareunia, or dysuria. Physical examination revealed no tenderness or palpable masses in the abdomen. Pelvic examination demonstrated a patent cervix and vagina with purulent discharge and bulging of the right lateral vaginal wall (Fig. 1A). The discharge was cultured for Neisseria gonorrhoeae, Chlamydia trachomatis, and Trichomonas vaginalis, but the results were negative. Laboratory tests revealed leukocytosis (18,220/mm3), C-reactive protein level of 1.18 mg/dL, and normal renal function. Transvaginal ultrasound images revealed uterus didelphys with a hypoechoic heterogeneous cystic mass measuring 4.8├Ś5 cm behind the bladder. The right kidney was not visualized on subsequent renal ultrasound. Abdominopelvic MRI was performed to better identify the pelvic anatomy and verify the absence of the right kidney. This study confirmed the ultrasound findings of uterus didelphys with a distended right hemivagina measuring 3.1├Ś3.5├Ś4.8 cm (Fig. 2A), suggesting a turbid fluid collection (Fig. 2B), and right renal agenesis (Fig. 2C). The patient was diagnosed with HWWS complicated with pyocolpos. Resection of the vaginal septum was planned and prophylactic antibiotics were administered before surgery. Initially, a puncture was made into the right vaginal wall to identify the obstructed vaginal septum before the resection began. After confirmation of the septum, it was incised with electrocautery, and 200 mL of foul-smelling purulent material was drained (Fig. 1B). A specimen was sent for culture and sensitivity testing. The vaginal septum was widely excised until the cervix was reached (Fig. 1C). Laparoscopic exploration revealed uterine didelphys, powder-burn appearing endometriosis on the serosal surface of the uterus (Fig. 1D), and pelvic adhesions (Fig. 1E). The patient underwent laparoscopic ablation of the endometrial implants. Cultures from the specimen grew group B beta-hemolytic streptococcus, for which the patient was given a 7-day course of amoxicillin-clavulanate. She was discharged 2 days after surgery, having had an uneventful recovery.
Uterine anomalies can result from failure of the M├╝llerian ducts to fuse in the midline, to connect with the urogenital sinus, or to create the appropriate lumen in the upper vagina and uterus by resorption of the central vaginal cells and the septum between the fused M├╝llerian ducts [2,4]. Lack of fusion of the two M├╝llerian ducts results in duplication of corpus and cervix [5]. Occasionally, uterus didelphys is associated with an obstructed hemivagina and often with ipsilateral renal agenesis [6]. Renal agenesis on the side of the obstructed vagina can be explained by embryologic arrest at 8 weeks of pregnancy, simultaneously affecting the M├╝llerian (paramesonephric) and Wolffian (metanephric) ducts [3,7]. This unique clinical syndrome was first described as HWWS in 1971. Estimates of its incidence range from 0.1% to 3.8% [8,9].
HWWS is usually discovered during puberty. Symptoms vary depending on the uterovaginal relationship in individual cases. A 10-year review of this anomaly showed that most patients presented with dysmenorrhea (73%), a pelvic or paravaginal mass (71%), and an affected right uterus and vagina (63.5%) [10]. In the present case, the patient presented unusually with excessive mucopurulent discharge. Pyocolpos can occur in patients with HWWS due to secondary infection of retained menstrual blood in the obstructed hemivagina. The two vaginal cavities can communicate through a partially fenestrated septum, or the two cervices can communicate through a fistula [11].
A careful pelvic examination to identify the cervix and vagina is the key to the diagnosis of M├╝llerian duct anomalies. Sonography can detect uterine malformations, but MRI is the study of choice for HWWS. MRI provides more detailed information regarding the uterine contour, the shape of the intrauterine cavity, the continuity with each vaginal lumen, the character of the septum, and the nature of the fluid content, as well as associated aspects such as endometriosis, pelvic adhesions, or renal anomalies [12].
The optimal treatment is full excision and marsupialization of the obstructing vaginal septum so both uteri can drain through the patent vagina [2]. In cases of pyocolpos or hematocolpos, two-step surgery may be recommended. Otherwise, distention and stretching of the septal tissue may increase the risk of inadequate resection and possible postoperative stenosis [13]. Laparoscopy is not mandatory but can be helpful in confirming the diagnosis when radiologic imaging is inconclusive. In addition, as in the reported case, laparoscopy is useful in the diagnosis and treatment of endometriotic lesions and pelvic adhesions, caused by retrograde menstruation from the obstructed hemivagina.
Uterine anomalies have long been associated with pregnancy loss and obstetric complications, but affected women generally are not infertile. A retrospective study of 36 patients with HWWS over a 30-year period revealed that 87% of the patients wanting children had a successful pregnancy, 23% had abortions, 15% had preterm births, and 62% had full-term pregnancies, for an overall live birth rate of 77% [14].
To our knowledge, HWWS is rare and only 10 cases have been reported in Korea [15]. Moreover, there have been no reports discussing the rare complication of pyocolpos in HWWS. Pyocolpos can occur in HWWS patients due to secondary infection of the obstructed hemivagina and thus may be difficult to diagnosis. Although it is not very common, it is important for clinicians to be aware of this entity, since timely diagnosis requires a high index of clinical suspicion.
References
1. Gholoum S, Puligandla PS, Hui T, Su W, Quiros E, Laberge JM. Management and outcome of patients with combined vaginal septum, bifid uterus, and ipsilateral renal agenesis (Herlyn-Werner-Wunderlich syndrome). J Pediatr Surg 2006;41:987-992. PMID: 16677898.


2. Jindal G, Kachhawa S, Meena GL, Dhakar G. Uterus didelphys with unilateral obstructed hemivagina with hematometrocolpos and hematosalpinx with ipsilateral renal agenesis. J Hum Reprod Sci 2009;2:87-89. PMID: 19881156.



3. Cox D, Ching BH. Herlyn-Werner-Wunderlich syndrome: a rare presentation with pyocolpos. J Radiol Case Rep 2012;6:9-15.

4. Ballesio L, Andreoli C, De Cicco ML, Angeli ML, Manganaro L. Hematocolpos in double vagina associated with uterus didelphus: US and MR findings. Eur J Radiol 2003;45:150-153. PMID: 12536095.


5. Han B, Herndon CN, Rosen MP, Wang ZJ, Daldrup-Link H. Uterine didelphys associated with obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome. Radiol Case Rep 2015;5:327PMID: 27307842.



6. Purslow C. A case of unilateral h├”matokolpos, h├”matometra and h├”matosalpinx. BJOG 1922;29:643.

7. Smith NA, Laufer MR. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow-up. Fertil Steril 2007;87:918-922. PMID: 17320871.


8. Troiano RN. Magnetic resonance imaging of mullerian duct anomalies of the uterus. Top Magn Reson Imaging 2003;14:269-279. PMID: 14578774.


9. Nassif J, Al Chami A, Abu Musa A, Nassar AH, Kurdi AT, Ghulmiyyah L. Vaginoscopic resection of vaginal septum. Surg Technol Int 2012;22:173-176. PMID: 23315718.

10. Phupong V, Pruksananonda K, Taneepanichskul S, Tresukosol D, Virutamasen P. Double uterus with unilaterally obstructed hemivagina and ipsilateral renal agenesis: a variety presentation and a 10-year review of the literature. J Med Assoc Thai 2000;83:569-574. PMID: 10863905.

11. Dias JL, Jogo R. Herlyn-Werner-Wunderlich syndrome: pre- and post-surgical MRI and US findings. Abdom Imaging 2015;40:2667-2682. PMID: 25852048.


12. Del Vescovo R, Battisti S, Di Paola V, Piccolo CL, Cazzato RL, Sansoni I, et al. Herlyn-Werner-Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging 2012;12:4PMID: 22405336.



13. Jones HW, Rock JA. Te linde's operative gynecology. 11th ed. Philadelphia (PA): Lippincott Williams & Wilkins; 2015.
14. Sanghvi Y, Shastri P, Mane SB, Dhende NP. Prepubertal presentation of Herlyn-Werner-Wunderlich syndrome: a case report. J Pediatr Surg 2011;46:1277-1280. PMID: 21683238.


Fig.┬Ā1
(A) Bulging of the right lateral vaginal wall (arrow) with presence of one cervix (Cx). (B) Pus drainage occurring after the incision of the obstructed vaginal septum. (C) Wide excision of the vaginal septum until two separate cervices are reached. (D) Laparoscopic findings of uterine didelphys and endometriotic lesions on the uterine serosa (arrow) (E) Laparoscopic findings of thin band adhesions (arrow).

Fig.┬Ā2
Uterus didelphys with an obstructed hemivagina and ipsilateral renal agenesis. Coronal T2-weighted magnetic resonance image demonstrates (A) two separate uterine cavities (arrows) with two separate cervices (arrowheads). (B) Dilatation of right hemivagina (arrow) and high signal intensity fluid with internal debris (asterisk), suggestive of pyocolpos. (C) Absent right kidney (arrow).
-
METRICS

- Related articles in Obstet Gynecol Sci
-
Mesenteric hydatid cyst: An unusual presentation.2012 May;55(5)
A case of Herlyn-Werner-Wunderlich syndrome diagnosed in asymptomatic newborn.2012 December;55(12)




















