The efficacy of pre-delivery prophylactic trans-catheter arterial balloon occlusion of bilateral internal iliac artery in patients with suspected placental adhesion
Article information
Abstract
Objective
Prophylactic trans-catheter arterial balloon occlusion (PTABO) before cesarean section of placenta previa totalis has been introduced to prevent massive hemorrhage. The purpose of this study is to evaluate the clinical usefulness of PTABO in cases of suspected placental adhesion and to examine antepartal risk factors and perinatal outcomes in women with placental adhesion.
Methods
Between January 2012 and December 2015, 77 patients who had undergone ultrasonography for evaluation of placenta previa were enrolled in this study. Seventeen of these patients with suspected placental adhesion by ultrasonography and Pelvic MRI underwent PTABO before cesarean section and another 59 patients underwent cesarean section without PTABO. Antepartal risk factors and peripartum maternal and neonatal outcomes were compared between patients with PTABO and those without PTABO.
Results
More advanced maternal age, longer in gestational weeks at delivery, and more common previous cesarean section history were observed in the PTABO group. Placenta adhesion, abnormal Doppler findings, and frequency of transfusion were more common in the PTABO group. However there was no significant difference in estimated blood loss, hospital days, and neonatal outcome. It had occurred 3 cases of hysterectomy and 1 case of uterine artery embolization after cesarean section in the PTABO group.
Conclusion
Close surveillance of antepartum risk factors for placental adhesion using ultrasonography and pelvic magnetic resonance imaging is important to prevention of massive hemorrhage during cesarean section. PTABO before cesarean section might result in reduced blood loss and requirement for transfusion during the operation.
Introduction
Placental adhesion including accreta, increta, and percreta is a serious complication of pregnancy, associated with major adverse outcomes of pregnancy, including life-threatening maternal hemorrhage, large-volume blood transfusion, peripartum hysterectomy and maternal and neonatal morbidity and mortality [12]. However, over the last 50 years, the incidence has increased 10 fold with a reported rate of one case every 2,500 deliveries [134].
Because prenatal placental adhesion can be diagnosed before delivery using ultrasound and magnetic resonance imaging (MRI) [56], both maternal and neonatal outcomes can be improved in high-risk populations [7]. Prophylactic trans-catheter arterial balloon occlusion (PTABO) has been introduced for effective management of postpartum hemorrhage and in the effort to save the uterus [156].
The aim of the current study was to determine the clinical efficacy and safety of prophylactic internal iliac artery balloon occlusion in patients with placental adhesion compared with antepartal risk factors and peripartum maternal and neonatal outcomes between patients with PTABO and those without PTABO.
Materials and methods
Between January 2012 and December 2015, 77 patients who had undergone US for evaluation of placenta previa were identified during the prenatal period. Seventeen of these patients had suspected placental adhesion and had undergone pelvic MRI. All patients received counselling and gave informed consent. The patients were divided into two groups: one group had undergone a conventional cesarean section with placenta previa totalis (control group, n=59) and the other group had undergone PTABO and cesarean section with the same indication (study group, n=18). Of 18 patients in the PTABO group, 17 patients had confirmed placental adhesion on pelvic MRI (94.4%).
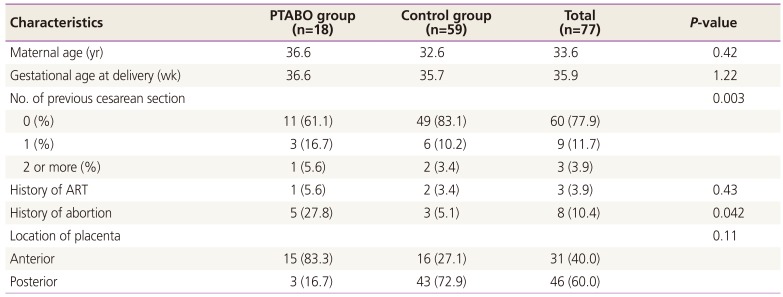
On ultrasonography, placental adhesion showed an irregular, thin uterine wall, prominent placental vessels and lacunae sign in placental spaces, and disruption of the bladder to the myometrial interface. Pelvic MRI showed uterine bulging, heterogeneous signal intensity within the placenta, dark intraplacental bands, focal interruptions to the myometrial wall, and invasion of pelvic structures by placental tissue in patients [28] (Fig. 1).
(A) Placenta lake and lacuna sign on ultrasonography and (B) uterine bulging sign on pelvic magnetic resonance imaging image in placenta adhesions.
Patients' demographic characteristics including number of cesarean sections, history of artificial reproductive techniques, placental location, presence of placenta previa, estimated blood loss during the operation, amounts of transfusion, intensive care unit (ICU) admission, stay in hospitalization, and peripartum hysterectomy were obtained from patient charts. Estimated blood loss was quantified using the volume of suction containers, weight of swabs, and visual estimation of vaginal blood loss. In cases of peripartum hysterectomy, placental adhesions including accreta, increta, and percreta were confirmed by pathological evaluation.
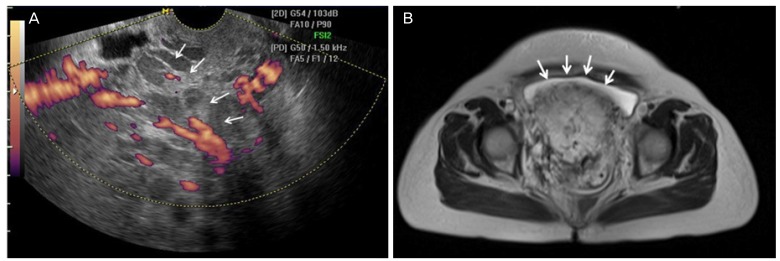
The internal iliac arteries were catheterized unilaterally and a guidewire was inserted with the distal end placed in the rear branch of the internal iliac arteries. Occlusion balloon catheters (5.5 Fr sheaths; Edwards Lifesciences, Unterschleissheim, Germany) inserted in both internal iliac arteries by a contralateral approach was achieved. Following insertion of the angiographic guidewire, a Monorail balloon catheter was introduced into the dissecting artery. Eleven millimeter of diameter of occlusion balloons were placed into the anterior division of the internal iliac arteries bilaterally, using pulsed low-dose fluoroscopic guidance to minimize radiation exposure [91011] (Fig. 2). The time of PTABO and operation was scheduled after full discussion with interventional radiology and anesthesiology the day before the cesarean section.

Angiography during prophylactic trans-catheter arterial balloon occlusion (PTABO). (A) Equipment in PTABO, (B) angiographic image after insert arterial catheter, and (C) posture of patient with PTABO.
Proceed of PTABO was collaborated with department of interventional radiology in intervention room, under local anesthesia by lidocaine injection. After the procedure, the patient transported from intervention room to operation room. To prevent dislocation of catheter, we moved patients very carefully from intervention radiology room to operation room.
All patients were underwent general anesthesia in principle, cooperated with department of anesthesiology shortly before cesarean section in operating room. Because, the operation processed in general anesthesia when the patient is infeasible changing of maternal position or need additional procedure such as peripartum hysterectomy because of severe placental adhesion.
Following delivery and umbilical cord clamping during cesarean section, temporary arterial balloon occlusion was performed prior to placental dissection. Following removal of the placenta, the blood vessels on the uterine wall were ligated during inflation of the balloon for at least 5 minutes, and hemostasis was then confirmed at the suture site after deflation of the balloon catheter for 1 minute. If bleeding continued after application of PTABO, uterine artery embolization (UAE) was performed after cesarean section, moving to the intervention radiology room from operating room immediately using the angiographic catheter prior to previous insertion status. If the patient's condition was unstable, the doctor of department of anesthesiology kept monitoring of the patient's condition during the procedure. Hysterectomy was performed after failure to control bleeding with PTABO and UAE [1213].
Statistical analysis was performed using paired t-test and chi-square test (PASW ver. 18.0, SPSS Inc., Chicago, IL, USA) and P<0.05 was considered clinically significant.
Results
Placental adhesion was confirmed by pelvic MRI in 17 of 18 patients (one emergent patient had not undergone MRI due to insufficient time.) who underwent PTABO and 10 cases were completed without additional procedures but 5 cases in UAE and peripartum hysterectomy was required in 3 cases of UAE. Of 59 patients with placenta previa totalis (as a control group) who underwent only cesarean section, additional procedures were required for management of postpartum bleeding such as UAE in 5 cases (Fig. 3).
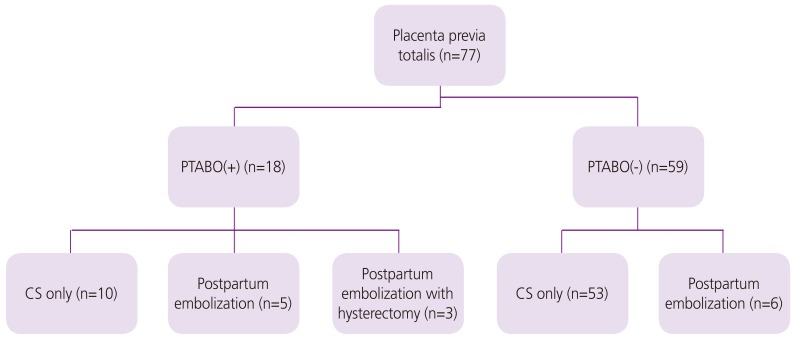
Patient distribution and management of placental adhesion. PTABO, prophylactic trans-catheter arterial balloon occlusion; CS, cesarean section.
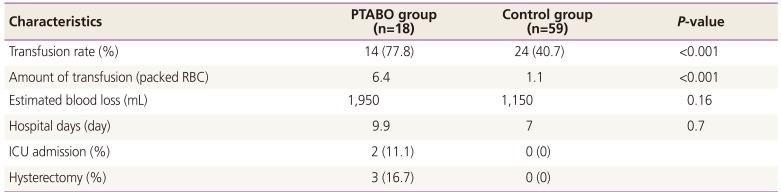
More patients in the PTABO group had a history of cesarean section and artificial abortion (P=0.003 and P=0.042). The anterior placental location was more common in the PTABO group compared with the posterior location of the placenta in the PTABO group (Table 1).
There were more common frequency of transfusion rate (P<0.001) and amount of transfusion (P<0.001) in the PTABO group, however there were no significant differences in estimated blood loss (P=0.16), hospital days (P=0.7), and neonatal outcome (Table 2).
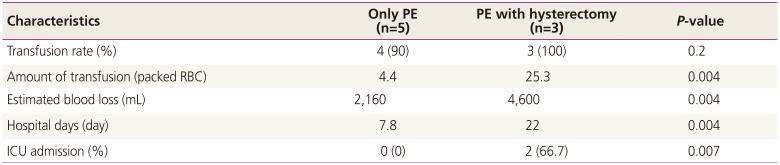
After UAE, bleeding had been continued, peripartum hysterectomy was undertaken. These grave cases in peripartum hysterectomy were uncontrolled move large amount of transfusion, amount of blood loss, more prolonged hospitalization and more frequent incidence of ICU care (Table 3).
Discussion
Antenatal diagnosis of placental adhesion reduced hemorrhage and the need for blood transfusion. This may be the result of differences in the management of antenatally diagnosed and undiagnosed women [514]. There are three recognized variants of abnormally invasive placentation: placenta accreta, in which placental villi invade the surface of the myometrium; placenta increta, in which placental villi extend into the myometrium; and placenta percreta, where the villi penetrate through the myometrium to the uterine serosa and may invade adjacent organs, such as the bladder [2].
Imaging study is important for diagnosis antenatally, which revealed placenta lacunae, loss of clear space, disruption of bladder, myometrial interface, increased vascularity by ultrasonography and uterine bulging, heterogeneous signal intensity within placenta, dark intraplacental bands, focal interruptions to myometrial wall, and invasion of pelvic structures by placental tissue by MRI [46].
Howard TF reported reduced blood loss with UAE and a decreased risk of peripartum hysterectomy. In addition, earlier use of balloon occlusion among women with postpartum hemorrhage was associated with fewer occurrences of maternal morbidity [15]. However interventions such as UAE for diagnosis of placenta adhesion would not be routinely performed before development of postpartum hemorrhage in women. There are potential benefits to decreasing the risk of postpartum hemorrhage and hysterectomy by administering prophylactic intervention such as the PTABO. In clinical application of PTABO, the most difficult problem is moving patients with the balloon catheter from the intervention room of radiology to the operation room for cesarean section. Vinas MT reported 2 cases of patient migration to the balloon catheter during patient transfer to the delivery suite from the IR suite. In both cases, this was detected by fluoroscopy immediately prior to caesarean section and repositioned [6].
Our patients had undergone dissection of internal iliac arteries with insertion of a guidewire using fluoroscopic guidance and a Monorail balloon catheter was placed at the distal end of the arterial branch of the internal iliac arteries in the angiography room. After the PTABO procedure, all patients were transferred to the operation room for caesarean section and moving patients with balloon catheter was very difficult, requiring great care, particularly while moving the stretching cart to the operation table. Fortunately, in our study no women in the PTABO group underwent displacement of the balloon catheter or had failure of bleeding control due to dislocation of the balloon catheter. There was no occurrence of procedure related complications in the mothers and their infants. However, there are still important problems limiting use of the PTABO procedure in the management of placental adhesion diagnosed antenatally [1116].
Cali et al. [1] observed no improvement in the outcomes of women treated with PTABO, compared with the outcomes of women treated without PTABO. There was no significant difference in the amount of estimated blood loss between placental accreta and increta, and difference was observed only in volume of blood loss in percreta.
We have no data regarding intrapartum and peripartum outcomes of suspected placental adhesion antenatally without PTABO, thus our study did not evaluate direct effects of PTABO. Our control group included patients with placenta previa totalis but not suspected placental adhesion by ultrasonography. The PTABO group included more grave cases including more patients with history of cesarean section and anterior location of placenta. With the exception of incidence of transfusion and amounts of transfusion, amount of blood loss, hospitalization days, and incidence of ICU care did not differ from those of the control group. This result indicates that PTABO had some effect in reducing maternal morbidity during cesarean section in cases of placental adhesion. There were 3 cases of peripartum hysterectomy in the PTABO group but no occurrence in the control group. Postpartum UAE was required in 5 cases in the PTABO group (27.8%) compared with 6 cases in the control group (11.3%) after cesarean section.
All patients had placenta previa totalis underwent screening USG regardless placental adhesion had suspected women had ultrasound features such as multiple placental lake and lacunae sign underwent pelvic MRI and the PTABO (n=17). Eleven women were diagnosed placental adhesion in the control group. However, there was too small number of control group for significant comparison.
In our study, no difference of perinatal outcomes were detected between the PTABO group were confirmed placental adhesion (n=18) and the control group including placenta adhesion (n=11). Therefore, we included patients with placenta previa totalis in regardless of placental adhesion in control group. One case of peripartum hysterectomy and ICU care was performed in each group.
PTABO were underwent since 2013, the control group included cases of severe placental adhesion before PTABO started. The control group and PTABO group had no significant difference of frequency of hysterectomy and postoperative bilateral UAE, thus, it was considered the equality of severity was saved in this study.
The decision regarding transfusion in PTABO cases might be the result of bias in patients with placental adhesion. Another benefit in PTABO is saving time in performance of postpartum UAE using prior displacement of the angiographic catheter. Significantly less blood loss and incidence of transfusion rates was observed in women treated with postpartum embolization compared to the group without postpartum embolization if massive postpartum bleeding continued during caesarean section despite performance of PTABO [1718].
The main limitation of this study is the small number of cases and the large gaps in numbers between the PTABO group and the control group. We restricted the diagnosis of placenta adhesion clinically to women with preservation of the uterus, therefore we cannot be certain that all cases were pathologically defined placenta adhesion [192021].
The Diagnosis Related Group (DRG) payment system, which has been implemented about cesarean section in university hospitals of Korea since July, 2003. physicians are difficult to receive a reward about additional procedure except in the cesarean section in high risk patients such as women were diagnosed placenta adhesion.
As this study, payment system changes from DRG to fee-for-service system in high risk patients, can charge the patients for partial additional cost. Pelvic MRI for detecting placental adhesion underwent in pregnant women at 35 weeks before cesarean section excluding DRG payment system by separatively admission.
In conclusion, bilateral PTABO in both internal iliac arteries prior to elective caesarean delivery in patients with placenta adhesion in whom uterine preservation is planned leads to improved outcomes. If massive bleeding continued after cesarean section, both UAE can be performed immediately after PTABO, which further decreased the risk of maternal mortality and morbidity. This approach should be considered when recommending this practice in all women identified as having placenta adhesion.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.