Laparoendoscopic single-site radical hysterectomy for early stage cervical cancer
Article information
Abstract
Technical developments have made laparoendoscopic single-site (LESS) surgery increasingly more feasible for treating gynecological conditions, including cancer. However, complex surgeries such as radical hysterectomy have rarely been performed with single-port access because of technical difficulties. The majority of the difficulties are due to the inefficient retraction of tissue during dissection. Here, we report a detailed description of LESS radical hysterectomy plus pelvic lymph node dissection that was successfully performed in two patients with stage IB1 cervical cancer. We used our expertise with LESS to perform space development as much as possible before the ligaments were resected. The oncologic clearance was comparable to that of conventional laparoscopic radical hysterectomy.
Introduction
Laparoscopic surgeries are routinely used to perform gynecological operations and technological advances have enabled the use of laparoscopy in gynecological oncology operations [1]. Accumulating data have demonstrated the possibility of replacing conventional multiple port laparoscopy with single-site surgery for treating gynecological malignancies [2]. This evolving surgical approach is expanding due to improvements in the recovery time, and it is associated with a shorter hospital day, lower analgesic requirements, fewer complications and patient satisfaction with the cosmetic appearance [34].
Nonetheless, several concerns remain about the feasibility of this approach in complex surgical procedures. Radical hysterectomy is complex pelvic procedure that requires many space developments with the appropriate retraction of tissues. Without appropriate retraction, surgical procedures are difficult to perform, especially when using the laparoendoscopic single-site (LESS) approach with a limited number of hands. We present our experience with single-port access laparoscopic radical hysterectomy with pelvic lymph node dissection in two patients with stage IB1 cervical cancer. The possibility and feasibility of using this technique to treat gynecological malignancies will be discussed.
Case report
1. Case 1
A 35-year-old, G2, P2 woman's condition was diagnosed as stage Ib1 cervical cancer after initial staging workup was performed, which included abdomino-pelvic magnetic resonance imaging and computed tomography examinations. Her body mass index was 20.02 kg/m2, and she had no medical or surgical history. Magnetic resonance imaging findings showed no pelvic or para-aortic lymph node metastases. The levels of the tumor markers including the serum squamous cell carcinoma antigen (normal range, 0 to 1.5), carcinoembryonic antigen and CA 125 were within normal range. Other preoperative laboratory findings were also within normal range.
Preoperative antibiotics and venous thrombosis prophylasix were administered, bowel preparation was performed and sequential compression devices were applied. Preoperative Foley catheter drainage was maintained during surgery and the RUMI uterine manipulator (Cooper Surgical, Trumbull, CT, USA) was used. During laparoscopy, no adhesion was seen, the uterus and both adnexa were grossly normal, and no enlarged pelvic lymph node was noted. The operative time was 180 minutes, and blood loss was 600 mL. Results of the pathology report showed an adenosquamous carcinoma, size 0.5×0.3 cm, and no parametrial invasion. Fourteen pelvic lymph nodes were resected.
The patient was discharged on the sixth day postoperatively. The Foley catheter was removed on the fourteenth day in the outpatient clinic, and the patient's bladder function recovered completely after removal. She was followed up in the outpatient clinic for more than 3 years without any evidence of recurrence or complications.
2. Case 2
A 60-year-old woman had early stage cervical cancer. Her body mass index was 23.29 kg/m2. She was being treated for hypertension and diabetes, and she had no surgical history. Magnetic resonance imaging findings showed no pelvic or para-aortic lymph node metastases. The serum squamous cell carcinoma antigen level was 0.4 ng/mL. The other preoperative laboratory findings were within normal range.
Preoperative antibiotics and venous thrombosis prophylaxis were administered and bowel preparation was performed in the same manner as aforementioned. Foley catheter drainage was performed, and the uterine manipulator was used. During laparoscopy, no adhesion was seen, the uterus and both adnexa were grossly normal, and no enlarged pelvic lymph node was noted. The operative time was 180 minutes, and blood loss was 200 mL. Results of the pathology report showed an adenosquamous carcinoma, size 1.2×1.0 cm; depth 0.9 cm with 1.2 cm of cervical wall invasion and no parametrial invasion. Twenty lymph nodes were resected.
The patient was discharged on the sixth day postoperatively, and bladder function successfully recovered on the fourteenth day postoperatively after the Foley catheter was removed. No complications for recurrence occurred for more than 3 years of follow-up.
3. Procedures
The patient was placed in the dorsal lithotomy position and the patient's left arm was tied to the body to provide space for the surgeon. The first assistant, positioned on the right side of the patient operated the surgical scope, and the second assistant, positioned between the patient's legs operated the uterine manipulator.
By using the open Hasson technique, a 2.5-cm vertical incision was made, and a wound retractor (Alexis, Applied Medical, Rancho Santa Margarita, CA, USA) was inserted transumbilically [5]. Once the wound retractor was fixed within the opening site, a surgical glove with sheaths inserted into three fingers was attached to the outer ring of the wound retractor and wound into a roll to maintain a pneumoperitoneum [678]. One of the advantages of using the surgical glove is that more space is available, especially during a complex surgery such as radical hysterectomy. The fingers of the glove function as a multiport for laparoscopic instruments and the camera. We used a rigid 0°, 5-mm laparoscope and articulating instruments (Roticulator, Covidien, Norwalk, CT, USA).
Following paravesical and pararectal space development, the uterine artery and ureter were identified (Fig. 1A). During this procedure, both posterior leaves of the broad ligaments were sutured and approximately retracted (Fig. 1B). The round ligament and anterior peritoneum were in situ during this procedure (Fig. 1C). Then the ureter was freed from the posterior leaf of the broad ligament down to the level where it entered the ureteral tunnel by using the Roticulator scissors (Covidien), and it was displaced laterally from the rectal pillar (Figs. 1D, 2A). The vesicocervical space was developed by using sharp dissection. Next, the ureter was completely and easily freed from the paracolpos easily because it was already dissected previously (Fig. 2B, C). The uterine artery was transected at its origin from the hypogastric artery. Following complete unroofing of the ureter, the rectovaginal space was developed. Then the uterosacral ligaments, cardinal ligaments, and portion of the paracolpos were divided by using the LigaSure device with a monopolar tip (Covidien), and the uterus was completely mobilized. Subsequently, the uterus was transected and removed vaginally under direct visualization around the cervix to ensure adequate margins. After removing the uterus, en bloc transperitoneal pelvic lymphadenectomy was performed. The external and common iliac lymph nodes were removed from the vessel surfaces by blunt or sharp dissection. The obturator fossa was entered and the obturator lymph nodes were removed. Lastly, the vaginal vault was closed vaginally (Fig. 2D).
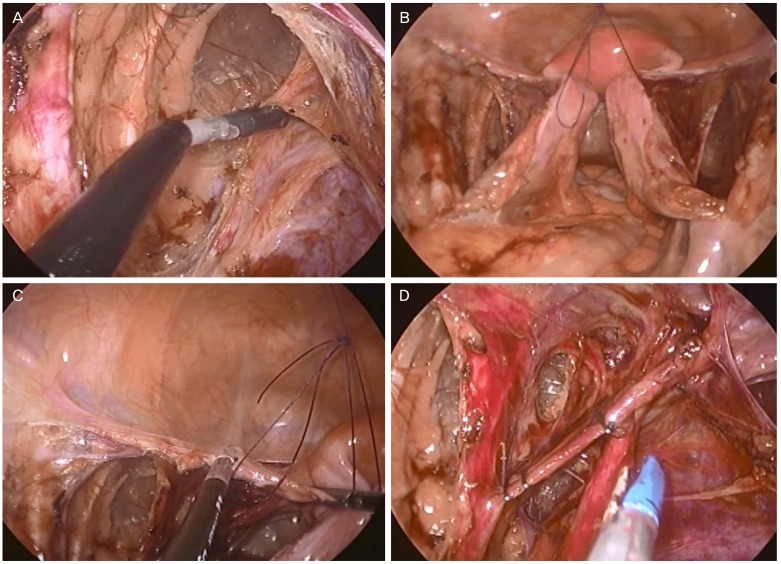
(A) Identification of the uterine artery and ureter. (B) Broad ligament suture for approximation. (C) Round ligament and anterior peritoneum in situ. (D) Lateral displacement of the ureter.

(A) Lateral displacement of ureter. (B,C) Ureter freed from paracolpos. (D) After pelvic lymphadenectomy and uterus removal followed by vault closure vaginally.
After bleeding was controlled, the wound retractor was removed. The transumbilical fascia was approximated with a 2-0 Polysorb suture (Covidien PLC, Dublin, Ireland), and the subcutaneous tissue was closed with a 4-0 Monosyn interrupted suture (B.Braun, Pfieffewiesen, Melsungen, Germany) interrupted suture. The skin was closed with a skin adhesive (Dermabond, Ethicon, Blue Ash, OH, USA) [5].
Discussion
With gradual advances in laparoscopic instruments and techniques, increasingly more single port laparoscopic surgeries are used in benign gynecological surgery. In gynecological oncology, simple hysterectomy and pelvic lymphadenectomy are performed with a single-site laparoscopic approach during the early stage of endometrial cancer. However, the procedure remains challenging for cervical cancer because of some of the limitations, including significant collisions between instruments. In the present patients, surgery was performed successfully with an adequate surgical margin, and the operative time was 180 minutes. Our operating times were not much longer than those of conventional laparoscopic radical hysterectomy, and this is partly because we have a lot of previous experience with single-port laparoscopic surgery for benign diseases. Also, the patients were disease free for 3 years postoperatively.
Single-site approaches have been successfully introduced for managing early stage cervical cancer. Technological advances during the past decade have facilitated the use of single-site surgery in gynecologic oncology surgeries, and the feasibility of performing radical hysterectomy plus pelvic lymph node dissection for early cervical cancer has been established. In single-port surgery, limited number of hands are available, so effective retraction methods are important. In our cases, the posterior leaves of the broad ligament were sutured for retraction. The round ligament, anterior peritoneum, and uterine artery were not cut during space development and dissection especially ureter tunneling which is one of the most difficult steps of radical hysterectomy. With these ligaments in situ and appropriate uterine manipulation, additional instruments for retraction can be omitted, which is important during single-port surgery.
The oncological outcome should be the top priority when managing gynecologic oncology patients. The present cases had a satisfactory outcome and no recurrence or complications. In conclusion, single-site radical hysterectomy plus pelvic lymphadenectomy is technically feasible and safe for treating gynecological malignancies. The role and advantage of single-port surgery in cervical cancer should be further evaluated in a larger number of patients.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
