|
 |
- Search
| Obstet Gynecol Sci > Volume 59(5); 2016 > Article |
Abstract
We describe a case of absent aortic and pulmonary valves, diagnosed at 16.4 weeks of gestation. Fetal echocardiography showed cardiomegaly with dilated both ventricles. No valve leaflets were observed in the aorta and pulmonary artery, and a typical to-and-fro flow pattern was noted in both great arteries on color Doppler imaging. Fetal hydrops was also detected. Follow-up ultrasonographic evaluation at 19 weeks demonstrated intrauterine fetal death. Postmortem autopsy revealed the absence of both aortic and pulmonary valve leaflets. To the best of our knowledge, this is the earliest diagnosed case of absent both aortic and pulmonary valves and only the second case to be diagnosed prenatally.
Congenital absent pulmonary valve (APV) is a rare anomaly occurring in about 0.2% to 0.4% of live born infants with congenital heart disease [1]. Absent aortic valve (AAV) is a much rarer cardiac anomaly with perhaps no more than two dozen reports in the literature [2], and a combination of these two conditions is extremely rare [3].
APV is characterized by absent, rudimentary, or dysplastic pulmonary valve leaflets. Echocardiographic findings of APV demonstrate a dilated right ventricle on four-chamber view and massive dilatation of main and branch pulmonary arteries on three-vessel view [4]. A color Doppler image shows a typical to-and-fro pattern of pulmonary stenosis and regurgitation. AAV may also demonstrate left heart dilatation with stenoinsufficiency similar to the characteristics of APV [2]. However, because of its rarity, prenatal echocardiographic findings have not been well described. Herein, we report a rare case of the absent both aortic and valves, which demonstrated a cardiomegaly with a typical to-and-fro flow pattern from both ventricles to both great arteries.
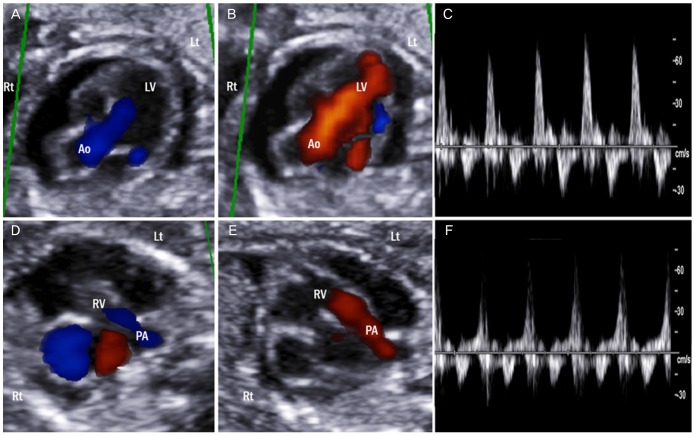
A 38-year-old multiparous woman was referred for detailed cardiovascular evaluation for cardiomegaly and pericardial effusion at 16.4 weeks of gestation. Her past medical and family histories were unremarkable. Sequential fetal screening testing indicated the risk for Down syndrome, but the fetal karyotype was not assessed. Ultrasonography demonstrated a singleton fetus with appropriate growth for gestational age. Generalized skin edema, bilateral pericardial effusion, and ascites were observed. Fetal echocardiography was performed, and a four-chamber view of the heart showed a cardiomegaly and ventricular septal defect (VSD). Both ventricles were dilated, and there were no discernible semilunar leaflets in either ventriculoarterial junctions. Color and pulsed-wave Doppler demonstrated typical to-and-fro flow across the annulus of both valves (Fig. 1). There were normal atrioventricular and ventriculoarterial connections, and no other abnormalities were detected.
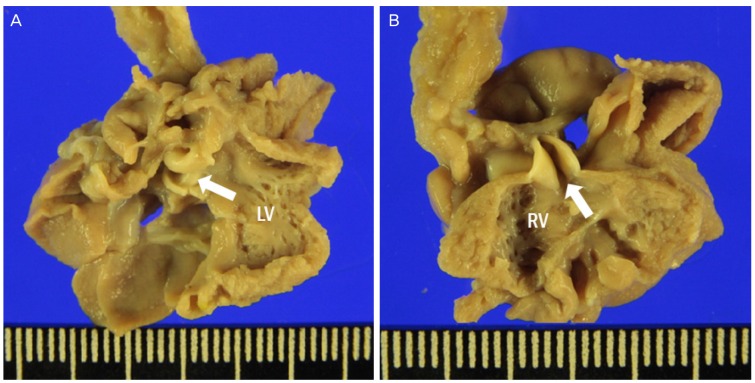
Following counseling on perinatal outcomes, amniocentesis for fetal karyotyping was recommended, but the parents declined. The woman revisited for a follow-up evaluation at 19 weeks of gestation and the fetus died. An abortus was delivered vaginally. Macroscopically, hydrops and nuchal fold thickening were observed. An autopsy confirmed the absence of both aortic and pulmonary valves with normally related great vessels (Fig. 2).
To the best of our knowledge, only five cases on the absence of both aortic and pulmonary valves have been reported to date [3,5,6], all in the 1990s. In four of those cases, fetal echocardiography could not be performed because of death in utero or induced abortion at 14, 18, 18, and 21 weeks of gestation, respectively, and therefore postmortem examination was used to confirm the condition [3]. Although prenatal diagnosis of both AAV and APV was feasible in the other case at 17.4 weeks, this case was reported in 1996 when ultrasonographic image quality was poor [6]. With advancements in fetal echocardiography, complex heart diseases can now be diagnosed with much higher accuracy even in early gestation. In our current report, we successfully diagnosed an extremely rare condition of the absence of both semilunar valves by advanced fetal echocardiography during early gestation.
APV and AAV are commonly associated with other cardiac anomalies. APV is mainly associated with tetralogy of Fallot, which is found in over 80% of APV cases, followed by VSD [5,7]. However, isolated APV may also develop. Although AAV has also been reported to be commonly associated with various cardiac diseases, such as double outlet right ventricle, VSD, and atrial septal defect, it can also present as an isolated finding [2]. However, a combination of APV and AVV has not been demonstrated previously as an isolated condition [2]. All reported cases to date were combined with other cardiac anomalies, most commonly with double outlet right ventricle, and extracardiac malformations. Our present case, however, showed APV and AVV in combination only with VSD, and there were no other additional extracardiac anomalies. From our report, we speculate that absence of both semilunar valves may present as an isolated finding, and therefore detailed fetal echocardiography is essential for diagnosing this condition.
The pathophysiology of the absence of both semilunar valves is unclear. Considering the common association of APV and AAV with conotruncal anomalies, such as tetraology of Fallot and double outlet right ventricle, as mentioned above, abnormal development of valve leaflets may be closely related to conotruncal evolution [5]. However, not all cases of absent both semilunar valves are associated with conotruncal anomalies, and APV and AAV can each occur as an isolated condition. Other mechanism such as maldevelopment of endocardial cusion at ventriculo-arterial junction have been suggested [3]. Genetic or environmental factors may also affect the underdevelopment of semilunar valves.
All reported cases of absent both semilunar valves resulted in fetal death or induced abortion because of fetal anomalies at around 18 gestational weeks [3,5,6]. Severe regurgitation across both great arteries leads to volume overload in both ventricles, causing fetal hydrops and death. Our present case also showed fetal hydrops with cardiomegaly at initial evaluation, and progressive cardiac failure may have resulted in fetal death. This may explain why postnatal manifestation of this condition has not yet been reported.
In conclusion, we report an extremely rare case of absent aortic and pulmonary valves, which was diagnosed at the earliest gestational age. This is also only the second known case to be prenatally detected. Careful echocardiographic examination can allow for a correct diagnosis even in early gestation.
References
1. Allan LD, Sharland GK, Milburn A, Lockhart SM, Groves AM, Anderson RH, et al. Prospective diagnosis of 1,006 consecutive cases of congenital heart disease in the fetus. J Am Coll Cardiol 1994;23:1452-1458. PMID: 8176106.


2. Murakami T, Horigome H, Shiono J, Ishiodori T, Ban Y, Gomi S, et al. Prenatal diagnosis of congenital absence of aortic valve: a report of two cases with different outcomes and a literature review. Fetal Diagn Ther 2015;38:307-314. PMID: 25170850.


3. Hartwig NG, Vermeij-Keers C, De Vries HE, Gittenberger-De Groot AC. Aplasia of semilunar valve leaflets: two case reports and developmental aspects. Pediatr Cardiol 1991;12:114-117. PMID: 1866330.


4. Abuhamad A, Chaoui R. Tetralogy of Fallot, pulmonary atresia with ventricular septal defect, and absent pulmonary valve syndrome. In: Abuhamad A, Chaoui R, editors. A practical guide to fetal echocardiography: normal and abnormal hearts. 3rd ed. Philadelphia (PA): Wolters Kluwer; 2016. p. 416-417.
5. Miyabara S, Ando M, Yoshida K, Saito N, Sugihara H. Absent aortic and pulmonary valves: investigation of three fetal cases with cystic hygroma and review of the literature. Heart Vessels 1994;9:49-55. PMID: 8113158.


6. Marek J, Skovranek J, Povysilova V. Congenital absence of aortic and pulmonary valve in a fetus with severe heart failure. Heart 1996;75:98-100. PMID: 8624884.



7. Wertaschnigg D, Jaeggi M, Chitayat D, Shannon P, Ryan G, Thompson M, et al. Prenatal diagnosis and outcome of absent pulmonary valve syndrome: contemporary single-center experience and review of the literature. Ultrasound Obstet Gynecol 2013;41:162-167. PMID: 22605612.


-
METRICS

-
- 4 Crossref
- 2,652 View
- 27 Download
- Related articles in Obstet Gynecol Sci
-
A case of prenatal diagnosed ectopia cordis by ultrasonography.1992 August;35(8)
A Case of Antenatally Diagnosed Cystic Adenomatoid Malformation of Lung.1998 July;41(7)
A Case of Antenatally Diagnosed Fetal Ovarian Cyst.1999 March;42(3)