Introduction
Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome is a malformation of the female genitals characterized by normal female phenotype, vaginal agenesis, a rudimentary or absent uterus and normal ovaries [1]. Oppelt et al. [2] further classified MRKH into typical, atypical, and MURCS (M├╝llerian duct aplasia, renal aplasia, and cervicothoracic somite dysplasia) associated types. The prevalence of MRKH is 1 in 4,000 to 1 in 5,000 women [3], and its association with inguinal ovaries is extremely rare. There are only few case reports of inguinal ovaries in MRKH syndrome and accompanying primary ovarian insufficiency is even more rarer [4]. The ideal management consists of surgical reduction of the gonads into pelvic cavity for the ectopic gonads and neovaginoplasty for vaginal agenesis. We present a case of MRKH syndrome with inguinal ovaries and ovarian dysgenesis in a young woman and review the clinicopathological findings in MRKH syndrome.
Case report
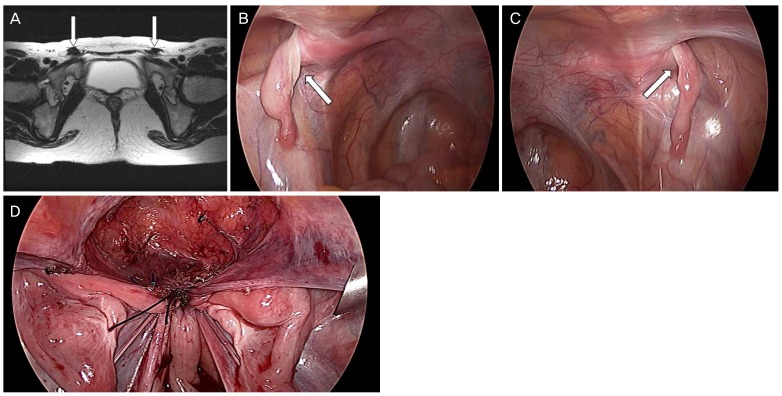
A 21-year-old woman was referred to out center for the evaluation of amenorrhea. She was 161 cm tall and weighs 50 kg. Physical examination showed normal secondary sexual characteristics except for the blind pouch of vagina. A transrectal ultrasonography and magnetic resonance imaging revealed atrophic inguinal ovaries (Fig. 1A-C), a single kidney and absence of uterus and cervix. The karyotype was 46, XX and serum basal hormone tests showed hypergonadotrophic hypogonadism status (follicle stimulating hormone 72.2 mIU/mL, luteinizing hormone 39.9 mIU/mL, estradiol 5 pg/mL, prolactin 0.1 ng/mL, antim├╝llerian hormone 0.08 ng/mL). Collectively, the diagnosis was MRKH associated with inguinal ovaries and primary ovarian insufficiency.
We performed neovaginoplasty using modified Davydov's procedure. After making a 1-cm vertical intra-umbilical skin incision, 10 mm trocar was inserted into the abdominal cavity for laparoscopic camera. A 10-mm and two 5-mm trocars were inserted into the lower abdomen. Laparoscopic exploration revealed two rudimental uterine horns and inguinal ovaries. A probe was inserted in the rectum to secure enough space between sigmoid colon and uterine horns. Meanwhile, an 8-cm-long vaginal mold (vagina dilator set; Vaginismus, Vaginismus.com, CA, USA) was inserted and pushed through the vaginal blind pouch to mark the vaginal opening.
About 4-cm transverse incision was made laparoscopically on the peritoneum below the connected rudimental uterine horns until the vaginal mold was exposed into the pelvic cavity to create vaginal opening. The pelvic peritoneum in the supravesical fossa was separated from the bladder. We then dissected both round ligaments and pulled the separated pelvic peritoneum out through the newly created vaginal opening. A purse string suture was performed through the bladder peritoneum, bilateral round ligaments, inguinal canals, tubo-ovarian ligaments, lateral sides of mesorectum, and rectosigmoid junction under the rectal mucosa using non-absorbable prolene 1-0 to make vaginal vault (Fig. 1D). Concomitantly we pulled the isthmus of the fallopian tube and tubo-ovarian ligament which was herniated in the inguinal canal to the pelvic cavity for making vaginal upper fornix
The remaining operation was completed vaginally. The pelvic peritoneum superior and inferior to the vaginal opening was pulled out into the vaginal cavity and it was repaired using monofilament 2-0 synthetic suture. At the completion of the surgery, the length of newly created vagina was 7 cm and the width was 3 cm. The vaginal mold inserted into the vaginal cavity thereafter until discharge.
We had the patient to keep the vaginal mold inserted for 24 hours at least for 3 days following the surgery. The patient was discharged from the hospital on the 7th day after the surgery without complications. We then limited the mold insertion only for 6 to 8 hours during the daytime and during the sleep. For the next first three months after the surgery, we asked the patient to keep the vaginal mold for 1 hour at least twice a day and maintain inserted overnight. After this period, we informed the patient to keep the mold only overnight until she is able to experience sexual intercourse without difficulties. Up to 12 months following the surgery, the patient continued to use vaginal mold and neovagina was shown to be intact (Fig. 2). Oral estrogen replacement was applied for the treatment of primary ovarian insufficiency.
Discussion
M├╝llerian agenesis or MRKH syndrome is a congenital malformation characterized by the failure of uterus and vagina to develop [3]. Most common clinical manifestations include uterovaginal aplasia or hypoplasia [5], and renal or skeletal malformation occurs only in 10% [6].
Genital hernia involving inguinal ovary is uncommon [7] and the co-occurrence of inguinal ovary with MRKH is even scarcer. Since the first case report by McDonough et al. in 1970 [8], the association between inguinal ovaries with m├╝llerian agenesis was well documented by a few case reports [9]. Strubbe et al. [3] reviewed 91 cases of MRKH syndrome and reported that only six patients had an inguinal ovaries. In rare incidences the hernia sac contained ovaries, fallopian tubes as well as uterus in MRKH syndrome [1,7,10].
At 7 to 8 weeks' gestations, the developing ovary is located on mesentery which forms the cranial suspensory ligament and the genitoinguinal ligament, or gubernaculum. The intra-abdominal portion of the gubernaculum ovary becomes attached to the lateral border of the uterus, evolving as the ligament of the ovary and the round ligament. As the m├╝llerian duct develops into the uterus, vagina and fallopian tubes, the ovaries remain close to the internal ring as an intraabdominal organ [11].
In inguinal genital hernia, the gubernaculum is proximally attached to the isolated uterine horn and distally to the external ring [11]. The incomplete closure of the processus vaginalis formed inside the gubernaculum contributes to the formation of inguinal genital hernia. The processus vaginalis and the round ligament can pass through the inguinal canal, causing inguinal hernia of ovaries, fallopian tubes, and even the uterus [1]. The indirect hernia in MRKH is considered to result from m├╝llerian abnormality, which comprises fusion defects of m├╝llerian ducts [10]. The hernia is suggested by an excess length and mobility of suspensory ligaments caused by the lack of fusion of the m├╝llerian ducts during the second month of fetal development [12].
Although inguinal ovary is well documented in MRKH, the ovary function in such cases has been underreported. In fact, most MRKH cases were presented with normal ovarian functions. Our patient however, showed hypergonadotrophic hypogonadism status (follicle stimulating hormone 72.2 mIU/mL, luteinizing hormone 39.9 mIU/mL, estradiol 5 pg/mL, prolactin 0.1 ng/mL, and anti-m├╝llerian hormone 0.08 ng/mL) suggesting primary ovarian insufficiency. Ovarian dysgenesis with 46, XX is defined as a primary ovarian defect leading to primary ovarian insufficiency due to failure of development and resistance to gonadotropin stimulation [13].
The ovary in the inguinal canal is not at risk of compression of its blood supply but rather is at a significant risk of torsion and infarction [14]. The vulnerability of inguinal ovary to infarction suggests a possible explanation for the ovarian insufficiency observed in our patient. Therefore, surgical repositioning of the inguinal ovaries into the pelvic cavity should be undertaken as soon as possible to preserve ovarian function.
Despite the ovarian dysgenesis, our patient showed secondary sexual characteristics. The laparoscopy revealed small yet morphologically otherwise normal ovaries. We postulated that the ovary function may gradually deteriorate to allow secondary sexual characteristics to develop.
In this article, we reported a rare case of MRKH with inguinal ovary and primary ovarian insufficiency. Although an indirect ovary hernia in young girls is not a rare condition, it is rare in adults. In this patient, the m├╝llerian system failed to fuse and ovaries were descended into the inguinal ring. The anatomical anomaly in MRKH is corrected by surgical procedure. We successfully performed neovaginoplasty using modified Davydov's procedure and repositioned bilateral inguinal ovaries in the pelvic cavity. The modified Davydov's technique consisted of the laparoscopic procedure followed by vaginal approach [15]. Oral estrogen replacement was also applied for the treatment of primary ovarian insufficiency.
In conclusion, MRKH is a complex syndrome involving uterus, fallopian tubes and other organs such as skeleton or renal system. The treatment must be individualized considering patient's age, and should be aimed to correct not only the anatomical anomaly but also hormonal dysfunction in cases of ovarian insufficiency.