Perioperative and postoperative morbidity after sacrocolpopexy according to age in Korean women
Article information
Abstract
Objective
This study aimed to compare perioperative and postoperative morbidity of older and younger women undergoing sacrocolpopexy (SCP).
Methods
A retrospective study included 271 patients who underwent laparotomic SCP for symptomatic pelvic organ prolapse from November 2008 to June 2013 at our institution. By the review of medical records, perioperative and postoperative data including the length of the surgery, estimated blood loss, blood transfusion, the length of hospital stay, wound complications and febrile morbidity were collected. In addition, cardiovascular, pulmonary, gastrointestinal, genitourinary, or neurological adverse events were retrieved. The need for an indwelling urinary catheter or performance of clean intermittent self-catheterization, mesh erosion rate and the number of days required for each were included in the postoperative outcomes. For the outcome variable analyzed in this study, the patients was dichomotized into women aged 65 and older and those younger than 65.
Results
One hundred and thirty-five (49.8%) patients were younger than 65 and 136 (50.2%) were aged 65 and older. Older women had higher body mass index, vaginal parity and prior surgery for hysterectomy than younger women (P<0.05). And older women had higher baseline comorbidities, such as hypertension, diabetes, cardiac disease (P<0.05), and their American society of Anesthesiologist class was higher (P<0.001). In the perioperative and postoperative complication, older group showed no differences in most of the operation-related complication rates, but gastrointestinal complication rate. Also, mesh erosion rate was not found to be significantly different between the two groups at the last visit.
Conclusion
Older women undergoing laparotomic SCP have similar perioperative and postoperative morbidities as younger women, suggesting surgeons can counsel older and younger women similarly in terms of operative risks.
Introduction
Korea is one of the most rapidly aging countries in the world. According to the recently released report by Korean government in 2013, the number of people aged 65 and over has been reached to more than 6 million and it consisted of 12.2% of total population. It also says that the number of people aged 65 and over will be reached up to 38.2% by 2050 in Korean society. The average life expectancy at the age of 65 has been growing and it was reported to reach 17.4 years in old man and 21.9 years in old women. It is generally well known life expectancy among women is longer than that of men. It is definite the burden of disease for the old women is demanding.
Pelvic floor disorders, including urinary incontinence, fecal incontinence, and pelvic organ prolapse (POP) are associated with aging process. Thus, they increase in incidence and prevalence with age. There is no doubt surgery is the most effective treatment modalities for POP [1,2]. In general, however, operative morbidity and mortality are known to be increased with age. For this reason, they are denied to be surgical candidates often. It is easily expected the number of women who suffer from POP is greatly increasing and older women can be the main beneficiaries of the surgery for POP. Under this circumstance, surgical outcome managing POP in older patients should be intensively discussed and the patients should be adequately counseled with age-specific data. But, there are few information in the literature mentioning risk-benefit of surgical treatment of POP in aged women, especially for the sacrocolpopexy (SCP). There is only one report about the effect of age on short-term outcomes after abdominal SCP for POP [3]. In this report, Richter et al. revealed that the outcomes of SCP were comparable between older and younger women except that older women had slightly longer hospital stays. However, in their report, preoperative stage was higher in older patients than younger patients. Therefore, we couldn't compare precisely the overall complications regardless of the stage in this study. Also, there has been no such research in Korean patients so far. Therefore, we aimed to compare perioperative and postoperative morbidity of older and younger women undergoing SCP.
Materials and methods
This study included 271 women who underwent SCP for symptomatic POP from the Department of Obstetrics and Gynecology, Seoul National University Hospital, from November 2008 to June 2013. It is a single center, retrospective and descriptive study. During the study period, all surgeries were done by one skilled surgeon. Demographic and background data including age, body mass index, American society of Anesthesiologist (ASA) class, comorbidities, preoperative POP-Q (pelvic organ prolapse quantification) stage were collected from the chart review. For the outcome variable analyzed in this study, the patients was dichotomized into women aged 65 and older and those younger than 65. Data including the length of the surgery and estimated blood loss were obtained intra-operatively. Immediate postoperative data collection include the length of hospital stay, blood transfusion (including intra-operative), wound complications and febrile morbidity. In addition, cardiovascular, pulmonary, gastrointestinal (GI), genitourinary, or neurological adverse events were noted. A foley catheter was inserted after anesthesia induction and was removed two days after SCP operation. Postoperative incomplete bladder emptying was defined in the presence of a failed first voiding trial 4 hours after catheter removal with a bladder volume of 200 cc or greater on nelaton catheterization in 2 consecutive trials. The need for an indwelling urinary catheter or performance of clean intermittent self catheterization and the number of days required for each were included in the postoperative outcomes. Postoperative mesh erosion rate was also compared. Perioperative and postoperative complications were retrospectively investigated through the review of medical records. The study protocol was approved by the institutional review board (H-1310-113-530).
The chi-square analysis was used for categorical variables and Mann-Whitney U-test was used for skewed data for continuous variables. Statistical significance was defined as P<0.05. Statistical analysis was performed using IBM SPSS ver. 19.0 (IBM Corp., Armonk, NY, USA).
Results
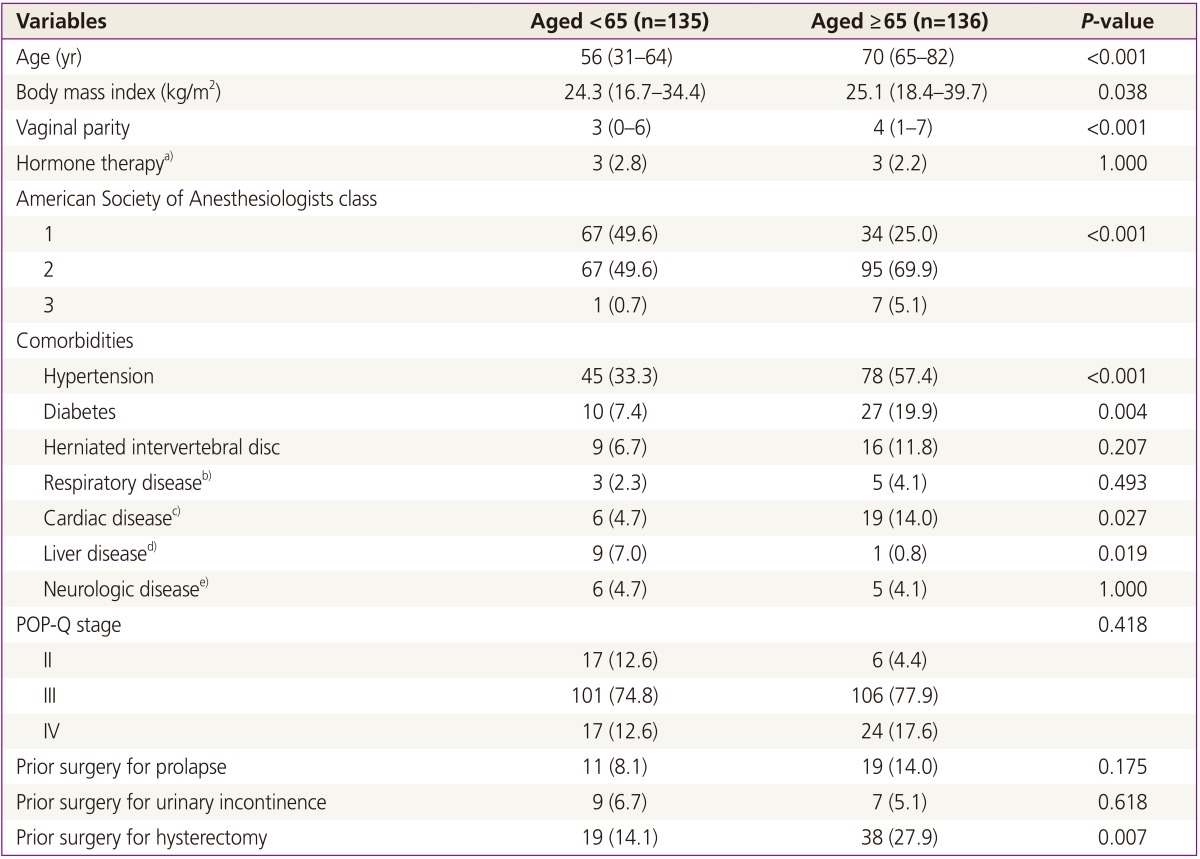
One hundred and thirty-five patients were younger than 65, and 136 were aged 65 and older. Table 1 displays baseline characteristics for both age groups. Median age of older group was 70 years old (range, 65 to 82 years). Older women had higher body mass index, vaginal parity and prior surgery for hysterectomy than younger women (P<0.05). And older women had higher baseline comorbidities, such as hypertension, diabetes, cardiac disease (P<0.05). In terms of baseline comorbidities, hypertension was the most common disease in both groups with 45 cases (33.3%) among the younger patients, and 78 (57.4%) among the older patients. Cardiac disease implied arrhythmia, valvular heart disease, coronary heart disease, old myocardial infarction and pericardial effusion in our cohort. In reflection of these higher underlying comorbidities, ASA class was also higher in older women (P<0.001). In our cohort of elderly women aged 65 and older, 95 patients (69.9%) were assigned at ASA class 2, 34 (25.0%) were ASA class 1 and 7 patients (5.1%) were class 3. None of the older patients were classified ASA class 4. Among younger women, 67 (49.6%) were ASA class 1 and 67 (49.6%) were assigned to ASA class 2.
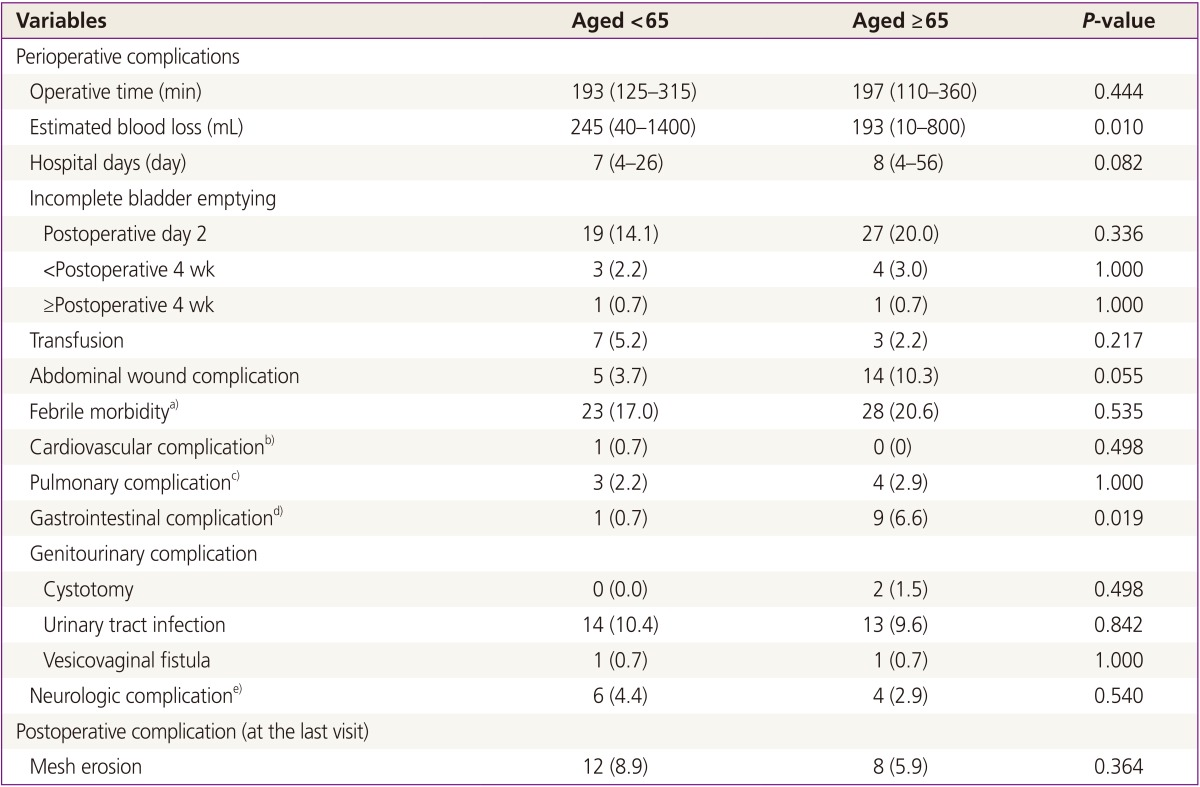
Table 2 shows perioperative and postoperative complication rates in both age groups. Operative time, transfusion and the length of hospital stay were not significantly different between the groups. In regard to the perioperative and postoperative complication rates, there were no differences between both groups in most variables. Only GI complication rate demonstrated higher incidence in older women. GI complications included ileus, microperforation of bowel and incisional hernia. Nine (6.6%) were identified as having significant GI morbidity in older women, whereas 1 (0.7%) women was suffered from GI complication in younger group. Among nine patients with GI morbidity in older group, eight had a prolonged initial hospital stay or were readmitted for the management of postoperative ileus. They recovered with medical treatment and discharged without further problems. The other one patient with small bowel obstruction undertook reoperation during their initial hospitalization. This case was turned out to have panperitonitis due to microperforation unrecognized during the operation. This patient undergoing small bowel segmental resection, end-to-end anastomosis, and ileostomy received ileostomy repair at postoperative 5 months and incisional herniorrhaphy with small bowel adhesiolysis at postoperative 2 years.
It seems that more incomplete bladder emptying, genitourinary complication, abdominal wound complication, and febrile morbidity are observed in older aged group (Table 2). However, none of them showed statistical significance. Although it does not have statistical significance, more mesh erosion cases were found in younger patients rather than in older ones (8.9% versus 5.9%) at the last visit.
Discussion
The present study suggests that the laparotomic SCP for symptomatic POP in older women is feasible and safe. Although older women had higher ASA class and underlying comorbidities of hypertension, diabetes, cardiopulmonary disease in absolute number, there found no significance differences in postoperative cardiopulmonary complications, interestingly. Thus, we could assume that operation-related risks were not higher in elderly women compared to younger women. It is true that older people have higher prevalence of baseline comorbidities and it makes gynecologic surgeons reluctant to propose surgical modality as the first choice for the treatment of POP until these days. This higher rate of systemic diseases in elderly group may be the reason for the stereotype that perioperative and postoperative morbidity and mortality rates are higher in elderly patients. However, it does not seem to have adequate evidence. Elderly patients seem fairly tolerable in surgery almost as well as the younger ones and it is supported by this study. Although older group showed higher ASA class (P<0.001), there were no differences in most of perioperative and postoperative complication rates between the older and younger groups in our cohort. Only GI complications demonstrated higher incidence in older women. Whitehead and colleagues once analyzed the risk factors of GI morbidity after abdominal SCP and reported that women with older age have a higher risk for significant GI morbidity [4]. Our result was consistent to their one. The association of age and postoperative GI complications has been also found in other abdominal surgeries. The possible explanations for this result would be decreased GI motility, decreased mobility and decreased tolerance to narcotics in the old patients [5,6].
Abdominal SCP is one of the most skill-demanding and time-consuming methods dealing with POP. The average SCP operation time was approximately 200 minutes, and longer operation time is usually a risk factor of postoperative complication. However, our cohort showed similar complication rates between younger and older aged groups in most variables. Even the median length of hospital stay was similar in both age groups. As our study does, there has been increasing numbers of reports older patients should not be excluded in any types of surgical indications, not only on gynecologic operation, but also on other surgical parts [7]. Most of the authors say elderly patients can undergo surgery even in the ninth and tenth decade of their life and the perioperative morbidity and mortality have been decreased during the last decade thanks to the advances in anesthesia and surgical techniques and improvement in perioperative care [8,9,10]. They point out that thorough evaluation of the medical status and extensive discussion with the patient and her family regarding the possible risks and expected benefits are required. Furthermore, some reports demonstrated no significant difference in the mean hospital stay as our study did [11]. Although it is for the gynecologic oncological patients, Giannice et al. found no correlation between severe comorbidities and median hospital stay [7,12].
POP is a major health concern among elderly women because it makes seriously negative impact on women's quality of life. POP produces discomforts such as urinary and/or fecal incontinence, voiding difficulty, pain, poor hygiene, limited mobility and impaired sexual life. Kim and colleagues has been reported that the prevalence of any degree of prolapse would be more than 50% in Korean women [13,14]. Lifetime risk of having gynecologic surgery due to POP ranges 11 to 19 % [15,16], and it is significantly higher than that of gynecologic cancer. These emphasize the need for active discussion about the surgical correction of POP in older women. Several series demonstrated surgical treatment of POP in elderly group had great benefit on their quality of life and high satisfaction rate [17,18].
The highlights of our study include all the surgical procedure were abdominal SCP given by one experienced surgeon, which minimized the confounding factors on postoperative outcomes. Abdominal SCP is technically demanding and time-consuming procedure compared with other techniques dealing with POP. We also set control group of younger patients, include their data in analysis, which make it possible direct comparison between two groups.
There are some limitations to our study. Our study included patients who underwent laparotomic SCP only, and therefore the result is hard to be applied to those undergoing laparoscopic SCP. Another limitation of our study includes relatively short follow-up duration. It may underestimate the incidence of postoperative complications such as relapse of POP and/or incontinence.
In conclusion, older women undergoing laparotomic SCP have similar perioperative and postoperative morbidities as younger women other than GI complication rates, suggesting surgeons can counsel older and younger patients similarly in terms of expected risks. Old aged women are the main beneficiaries of the surgery for POP and they do not suffer more from perioperative and postoperative complications than younger women. On the basis of this kind of data, surgical approach can be the principle option for the management of symptomatic POP in older women.
Notes
No potential conflict of interest relevant to this article was reported.