Laparoscopic uterine artery occlusion before cervical curettage in cervical ectopic pregnancy: Safe and effective for preventing massive bleeding
Article information
Abstract
Cervical ectopic pregnancy is associated with high risk for massive bleeding conditions. Cervical ectopic pregnancy can usually be treated by methotrexate injection or surgery. We present 4 cases of cervical ectopic pregnancy that were treated successfully with different uterine-conserving methods. By comparing our experience of 4 cases managed in different ways, we found that laparoscopic uterine artery occlusion before cervical curettage is more effective method for preventing massive bleeding.
Introduction
Cervical ectopic pregnancy is highly associated with for massive bleeding and occurs in 1/8,600 to 1/12,400 pregnancies [1]. Predisposing factors for this condition includes previous dilation and curettage [2], use of Intrauterine devices, endometriosis, uterine fibroids, previous cesarian sections, and history of assisted reproductive technologies [34]. Cervical pregnancy is usually diagnosed using transvaginal ultrasonography that identifies the gestational sac and peritrophoblastic blood flow or embryonic heartbeat at the cervix level with empty uterine cavity [5]. Painless vaginal bleeding is reported in 90% of cervical pregnancies, and such bleeding is often massive [1].
Cervical ectopic pregnancy can be treated medically or surgically. Methotrexate (MTX) has become the first-line uterine-conserving treatment in stable women. MTX can be administered either with systemic or directly into the gestational sac alone [2]. However, in unstable patients, surgical removal of the ectopic pregnancy and bleeding control is preferred over medical treatment. Moreover, in the case of uncontrollable bleeding, even hysterectomy may be required.
If surgical curettage is planned, intraoperative bleeding can be reduced by using preoperative procedures such as uterine artery embolization (UAE) [678], laparoscopic uterine artery occlusion (LUAO), ligation of the uterine arteries at cervical branches, vasopressin injection, or cerclage of the internal cervical os to compress feeding vessels [9101112]. In addition, postoperative bleeding can be controlled using Foley balloon catheter for cervical tamponade.
We present 4 cases of cervical ectopic pregnancies treated in one university hospital. The medical charts for all 4 cases were reviewed, and all records and results were included from admission via the emergency room or outpatient department of obstetrics and gynecology to discharge from the hospital, follow-up at the outpatient clinic, even readmission after 6 months to 2 years. UAE was performed by one radiologist within Radiologic Intervention Clinic of Inje University Haeundae Paik Hospital, and cervical curettage was performed by 2 different surgeons in obstetrics and gynecology.
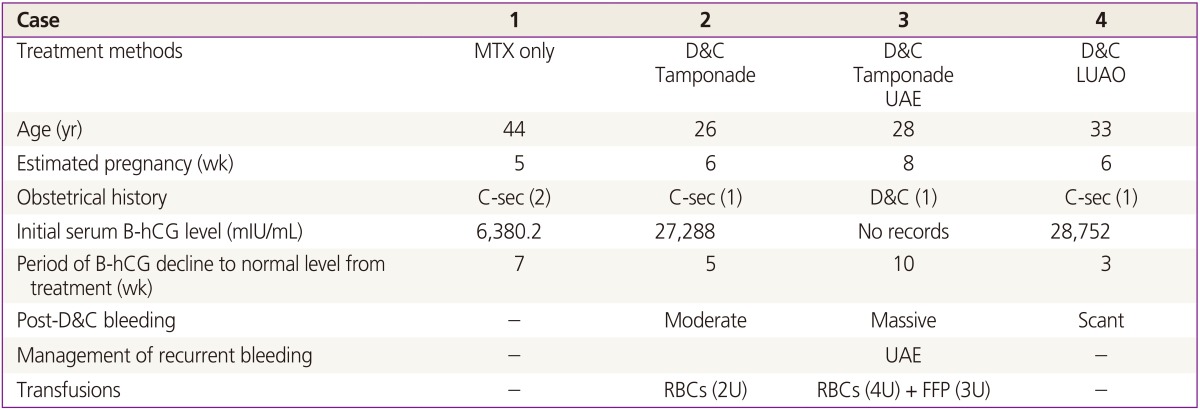
All cases were diagnosed using a pelvic examination, transvaginal ultrasonography, and serum beta-human chorionic gonadotropin (B-hCG) levels. Uterine-conserving surgical/medical treatment was performed in all patients, and no patients required hysterectomy, even during follow-up. Serum B-hCG levels were followed up until they reached normal levels (<10 mIU/mL). The methods of treatments, initial and follow-up serum B-hCG levels, amount of blood transfusions, recurrence of bleeding, needs for additional treatment, and complications for next pregnancy, of all four cases were compared. Demographic data for the 4 patients; obstetrical histories and characteristics are described in Table 1.
In 1 patient, only medical treatment was administered, and the other 3 patients underwent cervical curettage with postoperative cervical tamponade by using a Foley catheter. In each patient, the following different methods were used to prevent intraoperative bleeding: postoperative Foley catheter tamponade alone, preoperative and postoperative UAE, and pre-curettage LUAO. The pregnancies were at gestational 5 to 8 weeks, and the initial serum B-hCG levels ranged 6,380 to 28,752 mIU/mL.
Case report
1. Case 1
In this patient, systemic MTX was administered. The pregnancy was at gestational 5 weeks. Vaginal bleeding was observed, but vital signs were stable, and initial serum B-hCG level was 6,380 mIU/mL. MTX was injected intramuscularly, the dose of which depended on 50 mg/m2. For 1 week, mild vaginal bleeding persisted, and hemoglobin level decreased slightly to 11.1 from 12.1 g/dL. Serum B-hCG level decreased to <1.2 mIU/mL after 7 weeks.
2. Case 2
In this patient, cervical ectopic pregnancy was terminated surgically without prior preventive procedures. The pregnancy was at 6 weeks, and the patient's initial serum B-hCG level was 27,288 mIU/mL. After cervical curettage, a Foley catheter was postoperatively inserted into the endocervix. Intraoperative blood loss was >500 mL, and active bleeding was noted after curettage of the cervical ectopic mass. To control the bleeding, 2 Foley catheters were inserted for tamponade: a 20 Fr 3-way catheter with 30 mL ballooning and and 8 Fr catheter with 4 mL ballooning. A serial complete blood count was checked postoperatively. Hemoglobin levels decreased drastically, and two units of red blood cells (RBCs) were transfused in 1 day. After 24 hours, the Foley catheter tamponade was removed, and bleeding was minimal. Serum B-hCG level had decreased to normal by 5 weeks after the operation.
3. Case 3
In this patient, curettage of a cervical ectopic pregnancy and UAE were performed. The pregnancy was at gestational 8 weeks. Initial serum B-hCG level was unknown, but gestational sac with fetal pole and yolk sac were defined at the endocervical canal. After cervical curettage and UAE, Foley catheter inserted for tamponade. Intraoperative and postoperative blood loss was <100 mL, and hemoglobin level did not significantly decrease postoperatively (i.e., from 11.6 to 10.7 g/dL). Twenty-four hours postoperatively, the tamponade catheter was removed. However, 2 weeks later, the patient visited the emergency room with massive re-bleeding. Hemoglobin decreased to 6.7 g/dL, and vital signs were unstable. Emergency UAE and Foley catheter tamponade were performed, and 4 units of packed RBCs and 3 units of fresh frozen plasma were transfused. Serum B-hCG levels decreased gradually to 18.8 mIU/mL after 10 weeks. Although bleeding control and resuscitation were successful, but after 2 years, the patient was diagnosed with placenta previa totalis within her next pregnancy. Furthermore, she delivered at 28+5 weeks due to preterm premature rupture of membranes with massive bleeding, and emergency caesarian section was performed. Placenta previa totalis and placenta accrete were diagnosed intraoperatively caused massive bleeding. Postoperative bleeding was persisted, necessitating Bakri balloon tamponade (300 mL) and additional emergency UAE. Postoperative intensive care unit care was needed, with extensive transfusions (11 pints of RBCs, 4 pints of fresh frozen plasma) were needed during hospitalization periods.
4. Case 4
In this patient, surgical curettage of a cervical ectopic pregnancy was performed after medical treatment failed. The pregnancy was at gestational 6 weeks, and initial serum B-hCG level was 28,752.5 mIU/mL. Although intramuscular MTX was injected once with dose of which based on a 50 mg/m2 body surface area, the patient's serum B-hCG level increased to 35,439 mIU/mL after 1 week. Vaginal bleeding persisted and increased. To surgically remove the ectopic mass and for bleeding control, LUAO was performed before cervical curettage. Access to the uterine arteries on both right and left sides laparoscopically, and hemostatic clips were applied (Fig. 1). After clipping both uterine arteries, cervical curettage was performed as usual. The estimated intraoperative and postoperative blood loss was 40 mL. After 24 hours, bleeding had stopped. After 1 week, serum B-hCG level decreased to 69.2 mIU/mL, and after 3 weeks, the levels reached 0 mIU/mL. Abnormal vaginal bleeding was not seen after surgery, until 3-month follow-ups.
Discussion
Cervical ectopic pregnancy is associated with high risk of massive bleeding preoperatively, intraoperatively, and postoperatively because of rich blood supplies. The event occurs during reproductive years, and many patients wish to become pregnant again normally. Uterine-conserving treatment is needed, but high risk of bleeding makes difficult to treat these cases effectively. Therefore, lowering bleeding risk and effective removal of the ectopic pregnancy mass is the main challenge in these cases.
In case 1, treatment with systemic MTX was successful. However, serum B-hCG level declined gradually within 7 weeks, even though initial serum B-hCG level was lower than other cases. This case possibly had failed to resolve and continued to be at risk for bleeding, as observed in case 4.
The comparison between case 3 and 4 showed that performing UAE before cervical curettage in case 3 successfully controlled bleeding preoperatively, but B-hCG level declined for 10 weeks, and massive bleeding recurred during her next pregnancy, for which re-embolization for bleeding control and massive transfusion were needed. In addition, UAE and cervical curettage required at least 2 to 3 hours to be performed and treatments were given separately at different departments (Radiologic Intervention Clinic and the operation room).
This may be critical because of the time required. If the patient presents continuous bleeding, immediate surgical procedure is needed. In this respect, LUAO before cervical curettage as in case 4 was the better choice for time saving. UAE needs at least 45 to 60 minutes, and only could be performed by radiologic specialists at radiologic department [13]. But dilation and curettage after LUAO could be performed immediately in the operating room; no need for transfer and prepare separately, and able to anesthetize patient at a time. In LUAO, Bleeding was controlled as effectively as with UAE, and intraoperative and postoperative bleeding were not critical.
In case 4, postoperative serum B-hCG level declined much faster than in case 3. However, decline in serum B-hCG levels is a controversial way of measuring because cases 3 and 4 differed in terms of pregnancy week, initial B-hCG level, preoperative medication, and the surgeon's skills.
Both UAE and LUAO can be classified as "minimally invasive" methods that preserve fertility by preventing hysterectomy. Both methods are effective, but LUAO is considered a safer alternative to UAE (e.g., for lower risk of ovarian failure due to radiation) for treating uterine fibroids [131415]. Cramping pain due to uterine ischemia following UAE and LUAO is considerable. 30% of patients complaint in UAE, but none for LUAO in a previous comparative research [13]. Effectiveness of both techniques are similar, but in a bleeding state, LUAO could save time and reduce blood loss more effectively than UAE. Thus, if surgical treatment for cervical ectopic pregnancy is indicated, cervical curettage after LUAO could be the preferable surgical technique, because it is safe, effective treatment with good outcomes.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.