|
 |
- Search
| Obstet Gynecol Sci > Volume 58(4); 2015 > Article |
Abstract
Objective
To compare the intraoperative and postoperative outcomes of laparoendoscopic single-site surgery (LESS) versus conventional laparoscopic surgery in women with ovarian mature cystic teratoma.
Methods
A retrospective review of 303 women who underwent LESS (n=139) or conventional laparoscopic surgery (n=164) due to ovarian mature cystic teratoma was performed. Intra- and postoperative outcomes were compared between the two groups.
Results
There was no intergroup difference in age, body weight, height, body mass index, comorbidities, tumor size, bilaterality of tumor, or the type of surgery. However, more patients in the LESS group had a history of previous abdominal surgery (19.4% vs. 6.7%, P=0.001). Surgical outcomes including operating time (89 vs. 87.8 minutes, P=0.734), estimated blood loss (69.4 vs. 68.4 mL, P=0.842), transfusion requirement (2.2% vs. 0.6%, P=0.336), perioperative hemoglobin level change (1.3 vs. 1.2 g/dL, P=0.593), postoperative hospital stay (2.0 vs. 2.1 days, P=0.119), and complication rate (1.4% vs. 1.8%, P=0.999) did not differ between LESS and conventional groups. Postoperative pain scores measured using a visual analogue scale were significantly lower in the LESS group at 8 hours (P=0.021), 16 hours (P=0.034), and 32 hours (P=0.004) after surgery, and 32 of 139 patients (23%) in the LESS group and 78 of 164 patients (47.6%) in the conventional group required at least one additional analgesic (P<0.001).
Ovarian mature cystic teratoma is a benign tumor of the ovary comprised of ectodermal, mesodermal, and endodermal layers of germ cells. It is one of the most common ovarian tumors accounting for 25% to 40% of all ovarian tumors [1]. Although it can be discovered in postmenopausal women, more than 80% of ovarian mature cystic teratomas are diagnosed during reproductive years and it accounts for approximately 60% of all ovarian tumors in women younger than 40 years [2].
Laparoscopic ovarian cystectomy or salpingo-oophorectomy are the preferred surgical interventions for ovarian mature cystic teratoma [3,4,5]. Laparoscopic surgery has several proven advantages over open surgery in the management of ovarian mature cystic teratoma, including a significant reduction in operative morbidity, postoperative pain scores and analgesic requirements, hospital stay, and the recovery period [3,5]. Following its development for the surgical management of ovarian tumors, laparoendoscopic single-site surgery (LESS) is now showing increasing popularity [6,7,8,9,10,11,12,13,14,15,16,17,18]. It is thought that LESS may be an even less invasive surgical procedure than conventional multi-port laparoscopic surgery. However, it is uncertain whether LESS has comparable feasibility and postoperative outcomes to conventional laparoscopic surgery in the management of ovarian mature cystic teratoma. The aim of this study was to compare the intraoperative and postoperative outcomes of LESS versus conventional laparoscopic surgery in women with ovarian mature cystic teratoma.
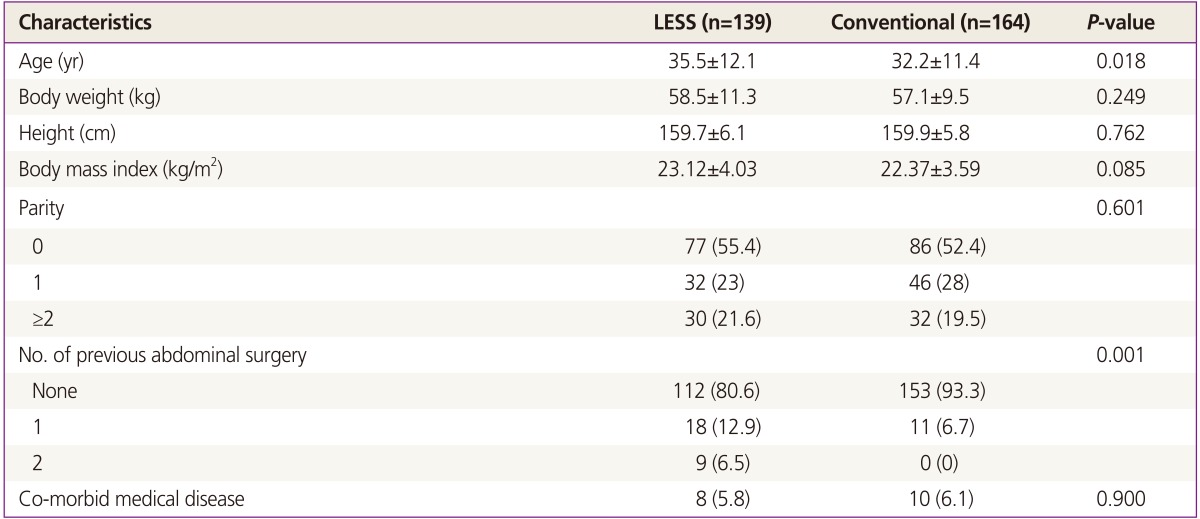
Following approval by the institutional review board of Asan Medical Center (Seoul, Korea), the medical records of 303 patients who were newly diagnosed with ovarian mature cystic teratoma and underwent laparoscopic surgery between 2009 and 2012 were retrospectively reviewed. A total of 139 patients underwent LESS and 164 patients underwent conventional laparoscopic surgery, and intra- and postoperative outcomes were compared between the two groups. Date was obtained from the patients' medical records as follows: 1) demographic data including age, body weight, height, body mass index, previous abdominal surgery, and comorbidities; 2) surgical data including tumor size, bilaterality of tumor, type of surgery, operating time, transfusion, perioperative hemoglobin level change, length of hospital stay, complications, postoperative pain score and analgesic use; and 3) postoperative outcomes including recurrence.
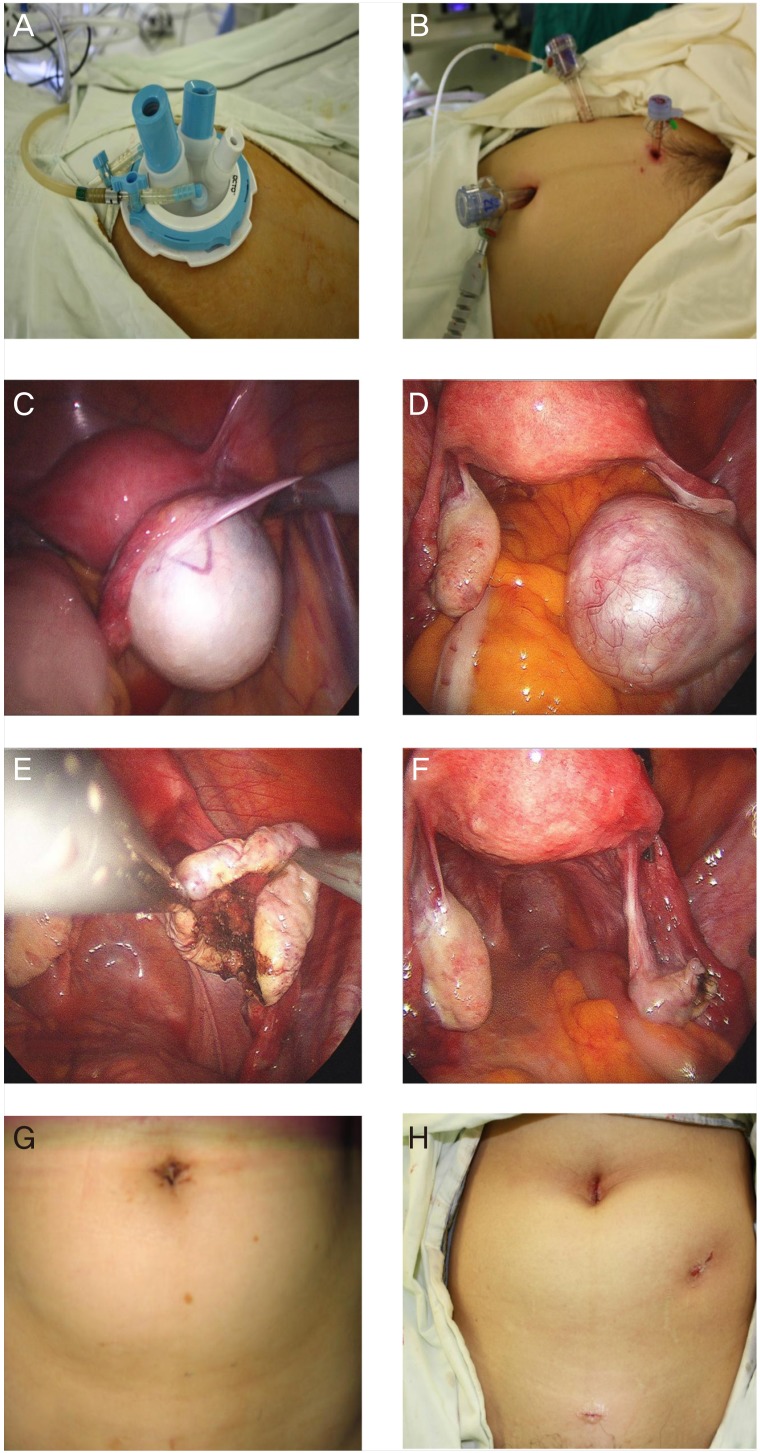
Under general anesthesia, patients were placed in the dorsal lithotomy, trendelenburg down position. A uterine manipulator (Cohen cannula) was placed through the uterine cervix for mobilization of the uterus and adnexal tumor during surgery. LESS was performed using a commercially available multichannel, single-port access system. After making a 1.5 cm longitudinal, linear skin incision at the base within the umbilicus, peritoneal access was obtained using an open Hasson technique Fig. 1. After inserting a multichannel, single-port access system through the umbilicus, pneumoperitoneum was created using CO2 gas at 8 to 12 mmHg. A 0 degree, 5 mm, rigid laparoscope was used. Surgeons stood on the left side of the patients and used the straight laparoscopic instruments with both hands. The first assistant (senior resident) stood on the right side of the patients and handled the laparoscope and the second assistant (junior resident) stood between the legs of the patients and handled the uterine manipulator. Salpingo-oophorectomy or ovarian cystectomy was performed as planned, and tumor specimens were extracted using endo-pouches. After surgery, the peritoneum and fascia was closed using 2-0 Vicryl suture and the skin was closed using skin adhesive. Operations were performed by multiple experienced laparoscopic surgeons. The selection criteria between LESS and conventional laparoscopic surgery were not clear. It was selected by the attending surgeon after discussion with patient.
Conventional laparoscopic surgery was performed using a three-port system. A 10, 12, and 5 mm trocar was placed using a closed technique on the umbilicus, left lower quadrant, and suprapubic area, respectively Fig 1. Except for the placement of laparoscopic ports, all aspects of the surgical techniques for LESS and conventional laparoscopic surgeries were identical.
Postoperatively, sips of water were allowed on the day of surgery and a normal diet was resumed on postoperative day (POD) 1. Postoperative pain was controlled with parenteral non-steroidal anti-inflammatory drugs (ketorolac, 10 mg) every 8 hours on the day of surgery and oral non-steroidal anti-inflammatory drugs (keotolac, 30 mg) every 8 hours from POD 1. Additional analgesics were given as requested with parenteral non-steroidal anti-inflammatory drugs. The pain score was measured using a visual analogue scale in 8 hours intervals and whenever the patients reported pain that required additional analgesics. A pain score of 0 was defined as "no pain" and 10 defined as "worst imaginable pain." Discharge was allowed when ordinary activities were resumed, pain was tolerable, and there were no symptoms or signs of complications requiring further treatment or reoperation from POD 1. Patients were followed up as outpatients 2 weeks and 1 month after surgery, and then every 6 months thereafter.
Mean values were compared using Student's t-test and frequency distributions were compared using the chi-square test or Fischer's exact test between groups. A P-value of <0.05 was considered to represent a statistically significant difference. Statistical analysis was performed using IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA).
The demographic characteristics of the two groups are compared in Table 1. There was no difference in age, body weight, height, body mass index and comorbidities between the two groups; however, more patients in the LESS group had a history of previous abdominal surgery.
The surgical outcomes are compared in Table 2. There was no difference in the mean tumor size, bilaterality of ovarian mature cystic teratoma, and the type of surgery between the two groups. No patient in either surgery group required an additional port or conversion to laparotomy to complete the planned surgery. The mean operating time (89.0 vs. 87.8 minutes, P=0.734) and estimated blood loss (69.4 vs. 68.4 mL, P=0.842) of the LESS group were comparable to the conventional laparoscopic surgery group. Three (2.2%) and one (0.6%) patient in the LESS and conventional group, respectively, required transfusion (P=0.336). The mean perioperative hemoglobin level change did not differ between the two groups (1.3 vs. 1.2 g/dL, P=0.593). The mean postoperative hospital stay was 2 days and 2.1 days for the LESS and conventional groups, respectively (P=0.119); however, more patients in the LESS group were discharged within 1 day of surgery (6.5% vs. 1.2%, P=0.026). Complications occurred in two (1.4%) and three (1.8%) patients in the LESS and conventional groups, respectively (P=0.999) (Table 2), but these were minor and managed conservatively. No patient required reoperation or readmission due to a complication. In the follow-up ultrasonogram, which was performed between 6 and 12 months after surgery, no patient in either group showed residual or recurrent ovarian mature cystic teratoma.
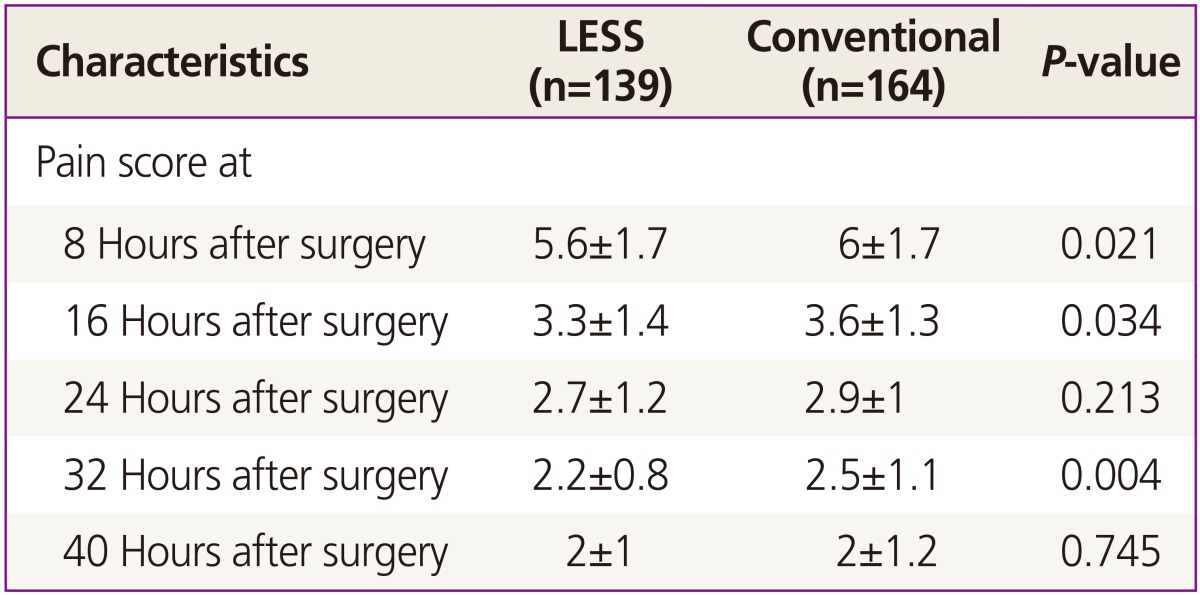
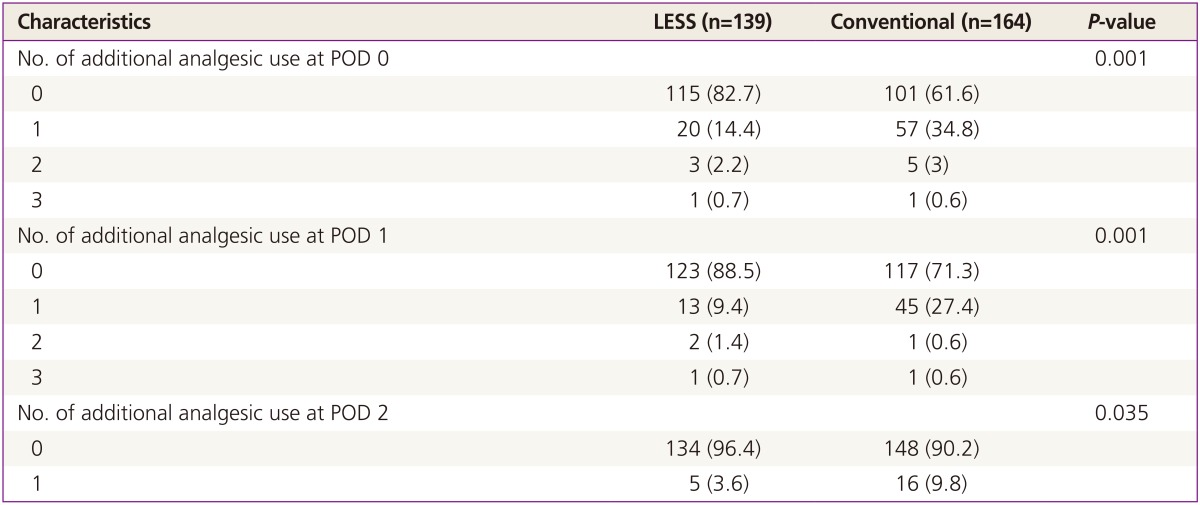
Postoperative pain scores between the two groups, as measured by a visual analogue scale in 8 hours intervals, are compared in Table 3. Pain scores were lower within 32 hours after surgery in the LESS group, and the differences were statistically significant at 8, 16, and 32 hours after surgery. Between surgery and discharge, 32 of 139 patients (23%) in the LESS group and 78 of 164 patients (47.6%) in the conventional group required at least one additional analgesic (P<0.001). The mean number of additional analgesics that were used in these patients was 1.7±0.8 and 1.7±0.8 (P=0.744), respectively. The use of additional analgesics on each POD was compared between the two groups in Table 4. Significantly more patients in the conventional group required additional analgesics at POD 0, 1, and 2.
Our results suggest that LESS is feasible in the surgical management of ovarian mature cystic teratoma because no patient required additional ports or conversion to laparotomy to complete the planned surgery. The surgical outcomes of LESS, including operating time, estimated blood loss, transfusion requirement, and postoperative hospital stay, were comparable to conventional laparoscopic surgery without increasing perioperative complications. However, the LESS group had a significantly lower postoperative pain score and analgesics requirement compared to the conventional group. Significantly more patients in the LESS group were discharged on POD 1. There was no intergroup difference in the recurrence rate of ovarian mature cystic teratoma.
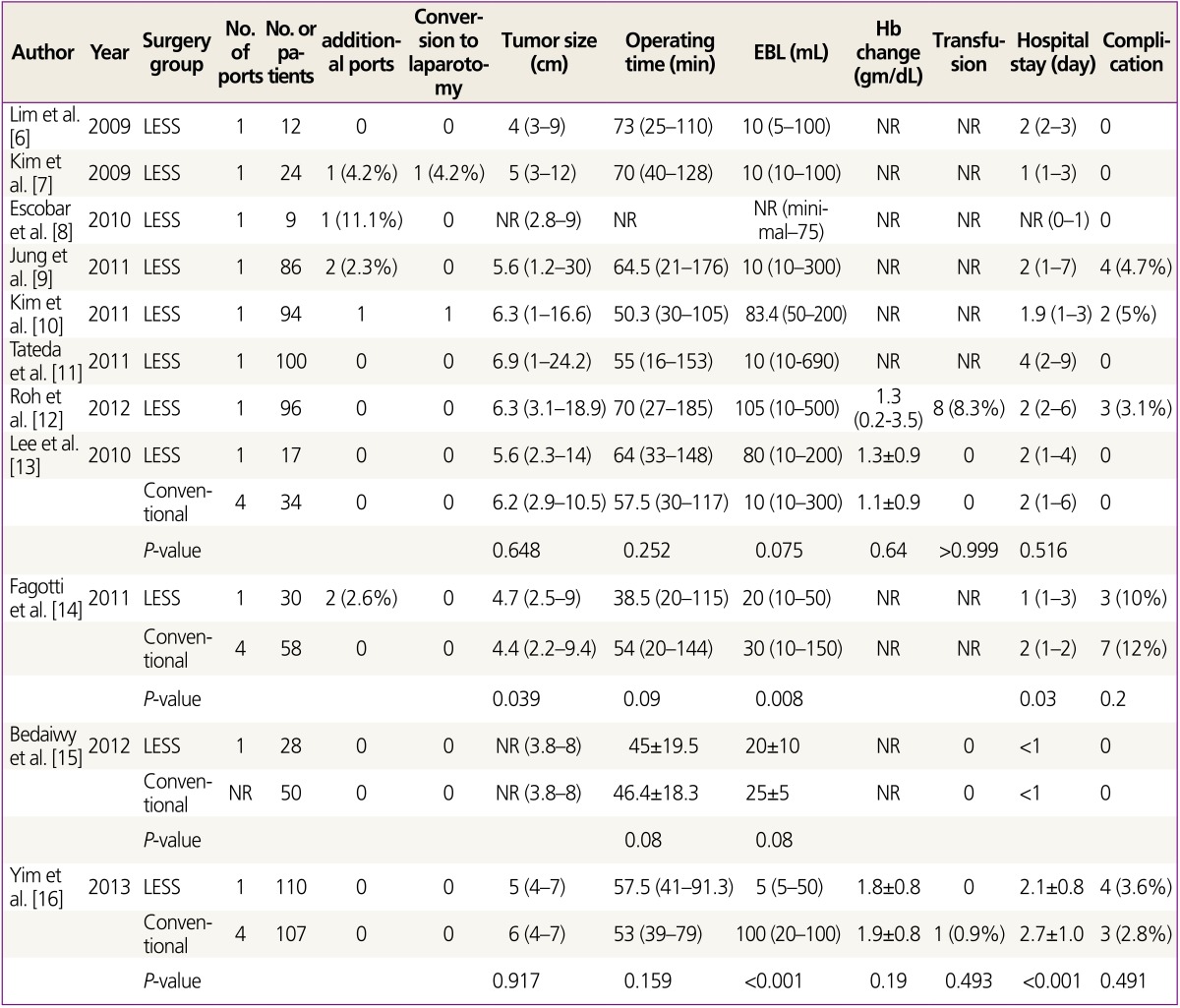
Pelosi and Pelosi [19] and Pelosi and Pelosi [20] first reported the use of LESS in gynecology in 1991, but it did not gain popularity for two decades. It is now showing increasing popularity in several surgical departments including gynecology, urology, general surgery, and chest surgery [21]. LESS lends itself well to ovarian mature cystic teratoma because it mainly occurs in adolescent or young women, in who the cosmetic outcomes of surgery are of great importance. Recently, several studies have reported the surgical outcomes of LESS for the management of ovarian tumors [6,7,8,9,10,11,12,13,14,15,16,17], but these reports included only small study populations and heterogeneous groups of ovarian tumors. The surgical outcomes specific to ovarian mature cystic teratoma have not been previously reported. To our knowledge, the present study, which focused on the surgical outcomes of LESS in the surgical management of ovarian mature cystic teratoma, is the largest case-control study on the outcomes of LESS in the surgical management of ovarian tumor (Table 5) [6,7,8,9,10,11,12,13,14,15,16].
Previous studies suggested that LESS was feasible for the surgical management of ovarian tumor. In the seven case series and four case-control studies that have been reported, a total of 640 patients underwent LESS surgery for ovarian tumor. Of these, seven patients (1.1%) required additional ports to complete the planned surgery due to adhesion (Table 5) [6,7,8,9,10,11,12,13,14,15,16]. Only three patients required conversion to laparotomy to complete the operation because the frozen-section pathology revealed malignant ovarian tumor [6,7,8,9,10,11,12,13,14,15,16]. In our series, no patient required an additional port or conversion to laparotomy; thus this study adds credence to the argument that LESS is feasible for the management of ovarian mature cystic teratoma.
In four previous case-control studies, the operating time of LESS was similar to that of conventional laparoscopic surgery (Table 5) [13,14,15,16]. Three of the four studies reported significantly less estimated blood loss in the LESS group, and two studies showed a trend towards shorter hospital stays for LESS patients. There was no difference in the occurrence of complications in these studies. In our series, the surgical outcomes of LESS were similar to those of conventional laparoscopic surgery, in agreement with previous studies.
In our series, postoperative pain scores measured by visual analogue scale were significantly lower in the LESS group, although the magnitude of the difference may have limited clinical relevance. It seems certain that LESS has advantages in postoperative pain because these patients had lower pain scores than the conventional group, despite receiving fewer analgesics. Two previous studies also reported that LESS patients required less analgesics than conventional laparoscopic patients [15,16]. Theoretically, postoperative pain is mainly of parietal origin, originating from incised skin, fascia, or muscle of the abdominal wall, which is in contrast to visceral pain, which originates from the peritoneal cavity. Therefore, the reduction in the abdominal incision in LESS may be associated with decreased postoperative pain.
Our study is limited due to its retrospective design and thus there is a possibility that bias may have been introduced. However, the demographic characteristics of patients were not significantly different between the LESS and conventional groups except age and the number of previous abdominal surgery. Although the mean age was younger for conventional laparoscopic surgery group, the difference of 3 years seems not clinically significant. A notable strength of this study is that it is the largest case-control study of LESS for ovarian tumors, and the first report on the surgical outcomes of LESS performed exclusively for treatment of ovarian mature cystic teratoma. We used three ports for conventional laparoscopic surgery in our study dislike previous studies which used four port for conventional laparoscopic surgery. Our study is the first one showing the reduced pain score which was measured using a Visual Analogue Scale in regular time intervals in LESS group after adenxal surgery.
In conclusion, LESS was feasible and showed comparable surgical outcomes with conventional laparoscopic surgery for women with ovarian mature cystic teratoma, with no increase in perioperative complications or recurrence after surgery. However, LESS was associated with less postoperative pain and required less analgesia.
References
1. Gordon A, Rosenshein N, Parmley T, Bhagavan B. Benign cystic teratomas in postmenopausal women. Am J Obstet Gynecol 1980;138:1120-1123. PMID: 7446619.


2. Koonings PP, Campbell K, Mishell DR Jr, Grimes DA. Relative frequency of primary ovarian neoplasms: a 10-year review. Obstet Gynecol 1989;74:921-926. PMID: 2685680.


3. Yuen PM, Yu KM, Yip SK, Lau WC, Rogers MS, Chang A. A randomized prospective study of laparoscopy and laparotomy in the management of benign ovarian masses. Am J Obstet Gynecol 1997;177:109-114. PMID: 9240592.


4. Mecke H, Savvas V. Laparoscopic surgery of dermoid cysts: intraoperative spillage and complications. Eur J Obstet Gynecol Reprod Biol 2001;96:80-84. PMID: 11311766.


5. Lin P, Falcone T, Tulandi T. Excision of ovarian dermoid cyst by laparoscopy and by laparotomy. Am J Obstet Gynecol 1995;173(3 Pt 1):769-771. PMID: 7573241.


6. Lim MC, Kim TJ, Kang S, Bae DS, Park SY, Seo SS. Embryonic natural orifice transumbilical endoscopic surgery (E-NOTES) for adnexal tumors. Surg Endosc 2009;23:2445-2449. PMID: 19343442.


7. Kim TJ, Lee YY, Kim MJ, Kim CJ, Kang H, Choi CH, et al. Single port access laparoscopic adnexal surgery. J Minim Invasive Gynecol 2009;16:612-615. PMID: 19835804.


8. Escobar PF, Bedaiwy MA, Fader AN, Falcone T. Laparoendoscopic single-site (LESS) surgery in patients with benign adnexal disease. Fertil Steril 2010;93:2074.e7-2074.e10. PMID: 20100614.


9. Jung YW, Choi YM, Chung CK, Yim GW, Lee M, Lee SH, et al. Single port transumbilical laparoscopic surgery for adnexal lesions: a single center experience in Korea. Eur J Obstet Gynecol Reprod Biol 2011;155:221-224. PMID: 21236555.


10. Kim WC, Lee JE, Kwon YS, Koo YJ, Lee IH, Lim KT. Laparoendoscopic single-site surgery (LESS) for adnexal tumors: one surgeon's initial experience over a one-year period. Eur J Obstet Gynecol Reprod Biol 2011;158:265-268. PMID: 21620559.


11. Takeda A, Imoto S, Mori M, Nakano T, Nakamura H. Isobaric laparoendoscopic single-site surgery with wound retractor for adnexal tumors: a single center experience with the initial 100 cases. Eur J Obstet Gynecol Reprod Biol 2011;157:190-196. PMID: 21470765.


12. Roh HJ, Lee SJ, Ahn JW, Kwon YS, Cho HJ, Kim DY. Single-port-access, hand-assisted laparoscopic surgery for benign large adnexal tumors versus single-port pure laparoscopic surgery for adnexal tumors. Surg Endosc 2012;26:693-703. PMID: 22038160.


13. Lee YY, Kim TJ, Kim CJ, Park HS, Choi CH, Lee JW, et al. Single port access laparoscopic adnexal surgery versus conventional laparoscopic adnexal surgery: a comparison of peri-operative outcomes. Eur J Obstet Gynecol Reprod Biol 2010;151:181-184. PMID: 20392556.


14. Fagotti A, Rossitto C, Marocco F, Gallotta V, Bottoni C, Scambia G, et al. Perioperative outcomes of laparoendoscopic single-site surgery (LESS) versus conventional laparoscopy for adnexal disease: a case. Control study. Surg Innov 2011;18:29-33. PMID: 21245066.


15. Bedaiwy MA, Starks D, Hurd W, Escobar PF. Laparoendoscopic single-site surgery in patients with benign adnexal disease: a comparative study. Gynecol Obstet Invest 2012;73:294-298. PMID: 22456304.


16. Yim GW, Lee M, Nam EJ, Kim S, Kim YT, Kim SW. Is single-port access laparoscopy less painful than conventional laparoscopy for adnexal surgery? A comparison of postoperative pain and surgical outcomes. Surg Innov 2013;20:46-54. PMID: 22410390.


17. Murji A, Patel VI, Leyland N, Choi M. Single-incision laparoscopy in gynecologic surgery: a systematic review and meta-analysis. Obstet Gynecol 2013;121:819-828. PMID: 23635683.


18. Lee IO, Yoon JW, Chung D, Yim GW, Nam EJ, Kim S, et al. A comparison of clinical and surgical outcomes between laparo-endoscopic single-site surgery and traditional multiport laparoscopic surgery for adnexal tumors. Obstet Gynecol Sci 2014;57:386-392. PMID: 25264529.



19. Pelosi MA, Pelosi MA 3rd. Laparoscopic supracervical hysterectomy using a single-umbilical puncture (mini-laparoscopy). J Reprod Med 1992;37:777-784. PMID: 1453397.

20. Pelosi MA, Pelosi MA 3rd. Laparoscopic hysterectomy with bilateral salpingo-oophorectomy using a single umbilical puncture. N J Med 1991;88:721-726. PMID: 1836254.

21. Romanelli JR, Earle DB. Single-port laparoscopic surgery: an overview. Surg Endosc 2009;23:1419-1427. PMID: 19347400.


Fig. 1
Laparoendoscopic single-site surgery (left) and conventional laparoscopic surgery (right) for ovarian mature cystic teratoma. Placement of ports (A,B). Ovarian mature cystic teratoma (C,D). Remained ovaries after ovarian cystectomy (E,F). Abdominal wounds after surgery (G,H).
-
METRICS

-
- 6 Crossref
- 3,036 View
- 31 Download
- Related articles in Obstet Gynecol Sci
-
A case of carcinoid tumor in ovarian mature cystic teratoma.2005 February;48(2)
A case of sarcoma arising in ovarian mature cystic teratoma.2007 October;50(10)