Introduction
Since the introduction of systemic chemotherapy in 1956 [
1], gestational trophoblastic neoplasia (GTN) has evolved into one of the most curable gynecologic malignancies. This has occurred primarily through sensitive assays for human chorionic gonadotrophin (hCG), advances in effective chemotherapy regimens, and the identification of risk factors that allow the individualization of chemotherapeutic treatment.
Although surgery has assumed a lesser role in the management of women with malignant gestational trophoblastic disease, selected surgical procedures remain important to treatment [
2]. Surgical intervention may be required for chemoresistant disease in the uterus or at metastatic sites, and for life-threatening complications such as hemorrhage, bowel or urinary obstruction, or infection [
3,
4,
5].
Patients with nonmetastatic or low-risk metastatic disease can be treated with single-agent chemotherapy [
2]. However, patients with high-risk GTN require multiagent chemotherapy, with additional surgery or radiation.
The objective of this study was to evaluate the role of adjuvant surgical procedures in the management of GTN.
Materials and methods
Between 1986 and 2006, 174 patients diagnosed with GTN were treated with chemotherapy at Severance Hospital. Patients were grouped according to the International Federation of Gynecology and Obstetrics (FIGO) stage and risk score. A FIGO risk score of ≥7 or the presence of one or more risk factors according to the clinical classification system was indicative of high-risk disease. Of the 174 patients, 129 (74%) were assigned to the nonmetastatic group; and 45 (26%), to the metastatic group. In the metastatic group, six patients were in the low-risk group and 39 were in the high-risk group. From this patient population, we identified 32 patients who underwent 35 surgical procedures as part of GTN treatment. The procedures included hysterectomy, pulmonary resection, craniotomy, uterine wedge resection, uterine suturing, salpingooophorectomy, pretherapy dilatation and curettage, adrenalectomy, nephrectomy, and uterine artery embolization.
Chemoresistant disease was defined as a plateau or increase in the level of hCG when the patient had achieved either a partial response (>50% decrease in hCG titers compared with the value at therapy initiation) or no response (≤50% decrease in hCG titers compared with the value at therapy initiation).
Results
Complete remission was achieved in all patients with non-metastatic and low-risk metastatic diseases and in 31 (79%) of the 39 patients with high-risk metastatic disease. However, 8 patients died.
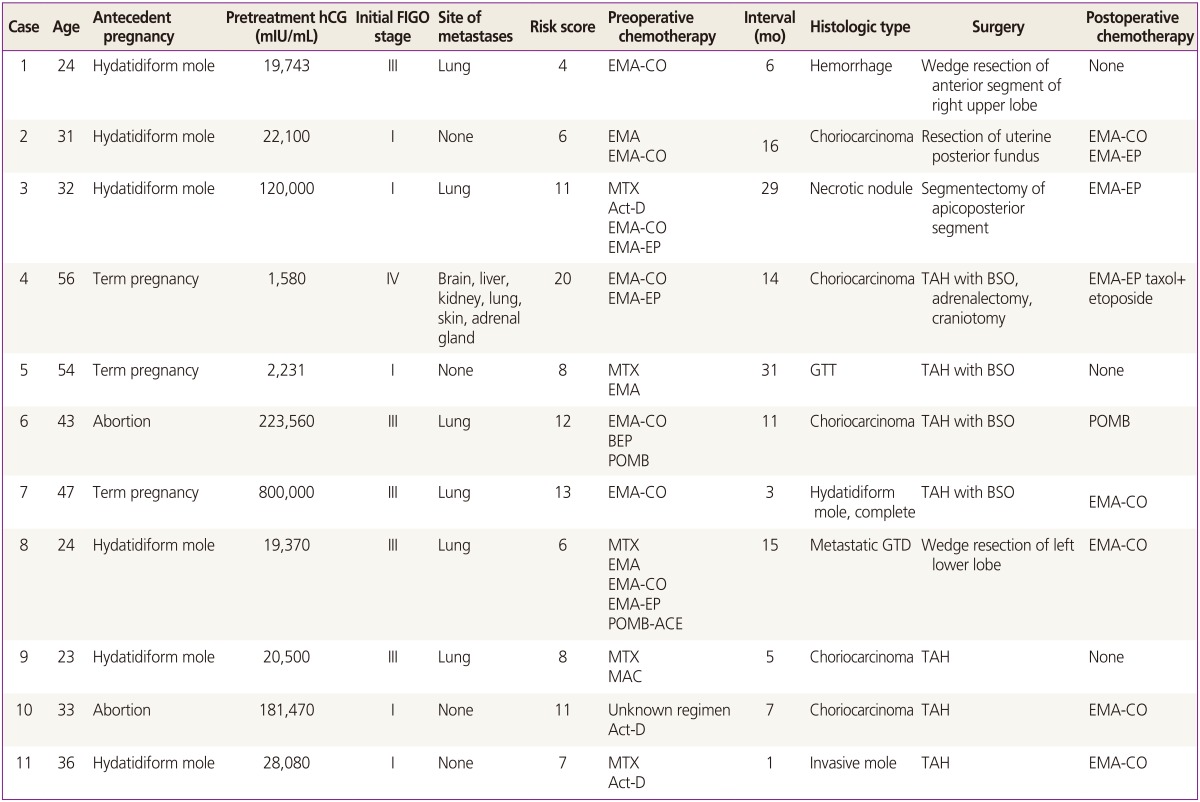
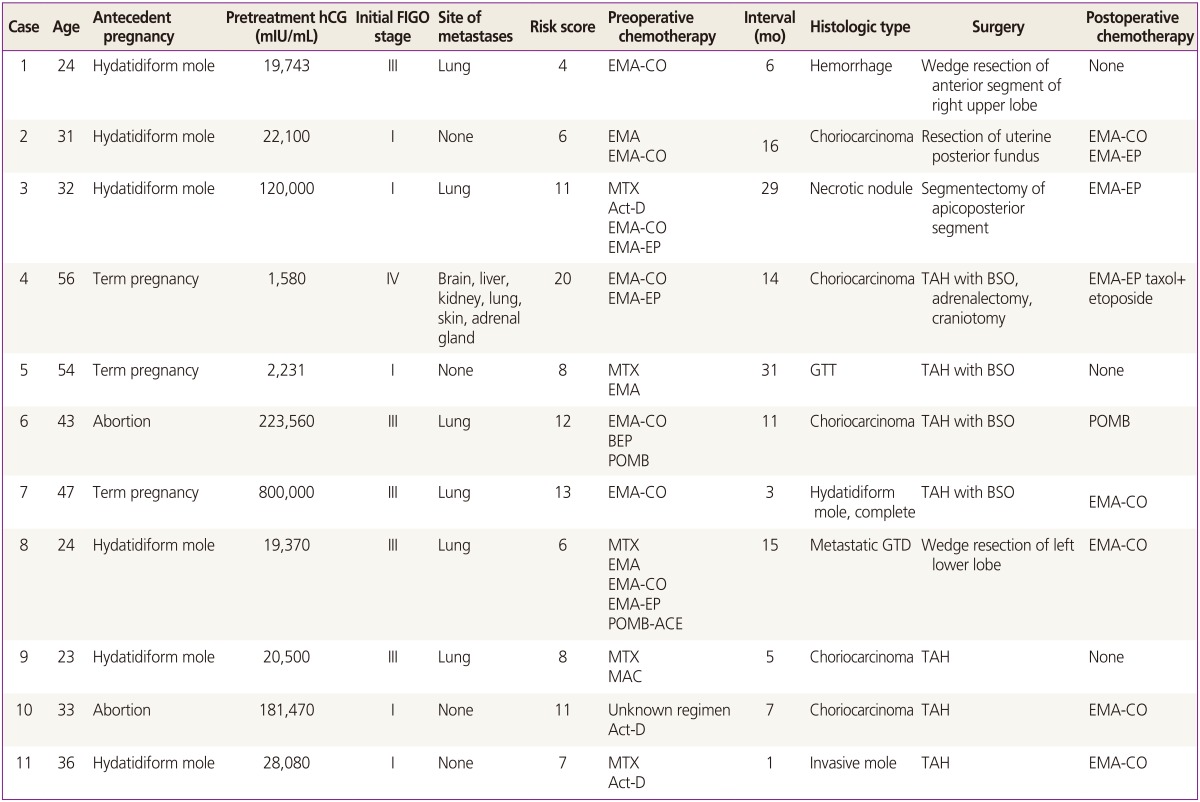
In 32 patients, 35 surgical procedures were performed. Two patients underwent more than one surgical procedure, including hysterectomy, adrenalectomy, craniotomy, hysterectomy, and uterine artery embolization. The presurgery characteristics of the 32 patients are presented in
Table 1. The median age of the patients at presentation was 36 years (range, 22 to 56 years). Thirteen patients had a pretreatment hCG level of ≥40,000 mIU/mL. Thirteen patients had an interval of ≥4 months from the antecedent pregnancy to treatment, 16 had an antecedent nonmolar pregnancy, and five had brain metastases. FIGO stage was I in 14, II in one, III in 12, and IV in five patients. In the metastatic group, two women were in the low-risk group and 15 were in the high-risk group. The FIGO prognostic risk factor scores ranged from 3 to 20 (median, 8.7). Twenty-one patients had risk scores ≥7. Pathology reports of surgical specimens identified 19 cases of choriocarcinoma, nine cases of invasive mole, two cases of hydatidiform mole, and two cases with nonviable trophoblast.
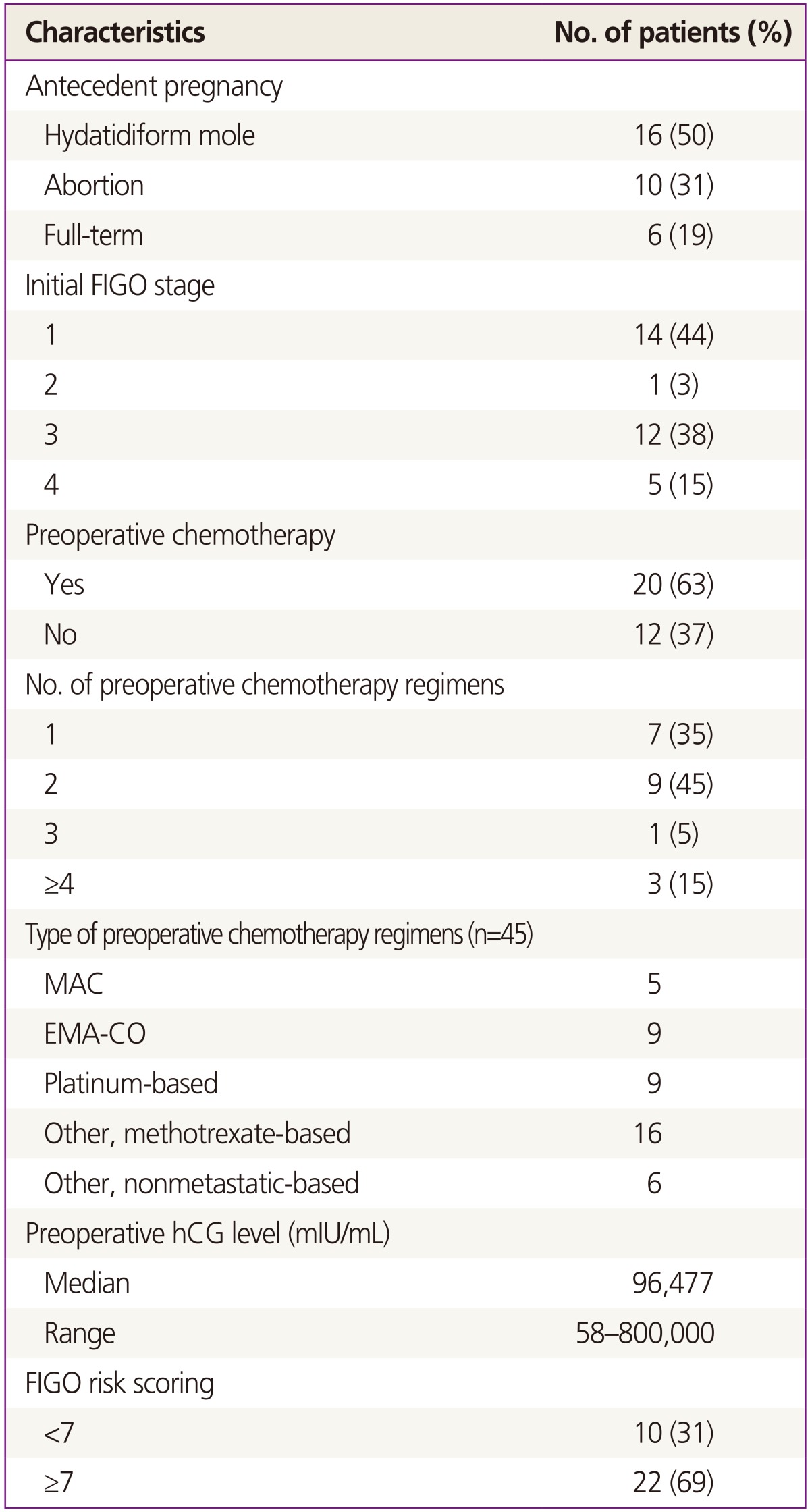
Twenty patients received preoperative chemotherapy. Before surgery, 45 different chemotherapy regimens were administered, including methotrexate, dactinomycin, and cyclophosphamide or chlorambucil regimens in 5 cases; etoposide, methotrexate, dactinomycin, cyclophosphamide, and vincristine regimens in 9 cases; platinum-based regimens in 9 cases; miscellaneous methotrexate-based regimens in 16 cases; and miscellaneous non-methotrexate-based regimens in 6 cases (
Table 1).
The surgical procedures and their indications are listed in
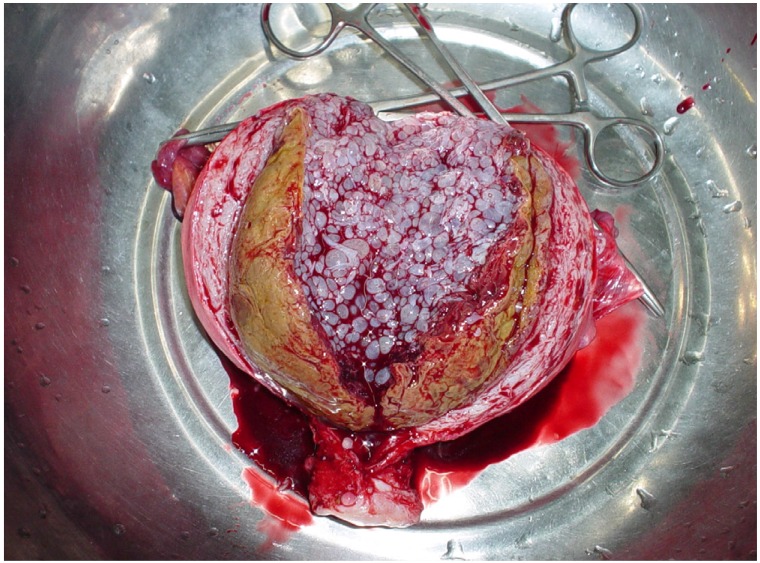
Table 2. Total abdominal hysterectomy was performed in 21 patients, lung wedge resection in 3 patients, and craniotomy in 4 patients. In selected patients, hysterectomy decreased the likelihood of postmolar GTN (
Fig. 1). Moreover, procedures such as uterine wedge resection, salpingo-oophorectomy, pretherapy dilatation and curettage, uterine suturing, adrenalectomy, nephrectomy, and uterine artery embolization were all performed once. After one or more chemotherapy regimens, 11 (34%) of 32 patients underwent surgery for chemoresistant disease. Of the 32 patients, 12 (38%) underwent procedures to control tumor hemorrhage. Five patients underwent procedures as adjuvant therapy at the start of chemotherapy. In addition, two patients underwent operations due to toxicity of chemotherapy.
Of the 32 patients, 28 (87%) who underwent surgical procedures survived. Four patients died, of whom one had stage III and three had stage IV disease, with FIGO scores of 12, 20, 14, and 10. Of the four patients who died, one died approximately 15 months after hysterectomy for chemoresistant choriocarcinoma. She had FIGO stage IV disease with brain, liver, kidney, lung, skin, and adrenal gland metastases. Left adrenalectomy was also performed for resection of resistant foci. Thereafter, she underwent craniotomy with tumor resection and removal of hematoma from acute hemorrhage, and stereotactic radiosurgery was performed after surgery. Another patient who experienced an intracerebral hemorrhage during chemotherapy underwent emergent craniotomy followed by postoperative chemotherapy and gamma knife irradiation, but eventually died of persistent disease. One patient had FIGO stage IV disease with brain and kidney metastases, and presented with hemoperitoneum. The patient was diagnosed with renal hemorrhage. Right nephrectomy was performed to control tumor hemorrhage. Afterward, the patient died of intracerebral hemorrhage while on ventilator support in the intensive care unit. The fourth patient died of chemoresistant disease, approximately 11 months after hysterectomy. She had undergone gastrectomy for stomach cancer; after hysterectomy, the pulmonary lesion aggravated, with the disease progressing despite postoperative chemotherapy.
Of 21 patients, 19 (90%) who underwent hysterectomy survived. All three patients who had resistant foci of choriocarcinoma in the lung achieved remission after pulmonary resection.
Five patients had brain metastases, all of whom also had pulmonary metastases. Craniotomy was performed in 4 patients. Emergent craniotomy with tumor resection and hematoma removal were performed for acute intracerebral hemorrhage. In three patients, postoperative multiagent chemotherapy was administered for choriocarcinoma diagnosed on surgical pathological examination. One patient received whole-brain radiation, and two patients underwent stereotactic radiosurgery after surgery. Complete remissions were achieved in two patients. Three of five patients with brain metastases died.
Table 3 shows the details of 11 patients who underwent surgery for chemoresistant disease after receiving one or more chemotherapy regimens. All patients had high-risk diseases. Of the 11 patients, 9 (81%) survived. Eight patients received further chemotherapy after surgical procedures. The median interval from diagnosis to surgery was 12 months. Of the seven women who underwent hysterectomies for resistant disease, three had nonmetastatic disease, three had lung metastasis, and one had multiple metastases, including the brain, liver, kidney, lung, skin, and adrenal gland. Of the seven patients, 5 (71%) also perioperatively received chemotherapy, five had complete remission, and two died of recurrent or persistent disease.
Pulmonary resection for removal of resistant foci of choriocarcinoma in the lung was performed in 3 patients, all of whom had complete disease remission after the operations. Uterine wedge resection was performed in one patient.
A pathological diagnosis of choriocarcinoma was made after salvage surgeries in 7 cases, and one case each of hydatidiform and invasive moles were also identified. Pathologically negative findings were obtained for two patients.
Discussion
Approximately half to two-third of patients with high-risk GTN need surgery during the course of therapy to remove disease or treat complications [
6,
7,
8]. Lewis et al. [
9] reported that the most common surgery was for hemorrhage control. With improvement in technology and development of other effective chemotherapeutic agents, the indications for surgery have changed. Currently, the most common surgical approach appears to be resection of chemoresistant foci of disease. In our series, surgery was most commonly performed for hemorrhage control in 12 cases, followed by salvage surgery for chemoresistant disease, which was performed in 11 patients.
Hammond et al. [
3] reported that patients with nonmetastatic or low-risk metastatic gestational trophoblastic disease who were treated with primary hysterectomy with chemotherapy had a shorter duration and lower total dosage of chemotherapy than patients who were treated with chemotherapy alone. Primary hysterectomy may be considered in selected patients with high-risk metastatic GTN with evidence of uterine disease. Delayed hysterectomy is often considered for patients who fail to respond to primary chemotherapy. In our study, 6 primary adjuvant hysterectomies were all performed for nonmetastatic disease, and the mean age of the patients was 47 years, which means that fertility preservation was not required. Five (71%) of 7 patients who underwent salvage hysterectomy for chemoresistant disease had complete clinical response to surgery.
Resection of pulmonary nodules in highly selected patients with drug-resistant disease may also be successful in inducing remission [
4,
10,
11,
12,
13,
14,
15,
16,
17]. Before performing pulmonary resection, it is important to rule out other concomitant diseases through extensive preoperative imaging. Tomoda et al. [
16] reported that 14 (93%) of their 15 patients with isolated, unilateral nodules associated with low urinary hCG values benefited from thoracotomy with pulmonary resection. Xu et al. [
18] noted improved survival in patients who had a solitary lung lesion without metastases to other organs and a good response to chemotherapy. In our study, all the three patients who met the above-mentioned criteria established by Tomoda et al. [
16] underwent pulmonary resection for chemoresistant disease and achieved complete remission.
Brain metastases of GTN tend to be highly vascular and develop central necrosis and hemorrhage. Thus, patients with brain metastases are at risk of early intracerebral hemorrhage, neurological deterioration, and early death. A combination of multiagent and whole-brain radiation therapies, treatment with early neurosurgical intervention or stereotactic radiosurgery, and combination chemotherapy with methotrexate systemic and intrathecal regimens have been reported to have similar cure rates as high as 75% [
19,
20,
21,
22]. Treatment with the combination of chemotherapy and whole-brain radiation therapy may be associated with late neurotoxicity such as impaired cognitive function. dementia, gait ataxia, and behavioral changes. Stereotactic radiation therapy allows precise delivery of a single high-dose fraction of radiation to a small target volume, with a sharp fall-off of the dose to adjacent normal tissues [
20]. In our study, four patients received emergent craniotomy with hematoma removal and tumor resection for acute cerebral hemorrhage, followed by postoperative chemotherapy and whole-brain irradiation in one and gamma knife irradiation in the other two patients. Two of the five patients with brain metastases survived without neurological sequelae. An interesting finding in our series concerns the use of postoperative chemotherapy. The patients who received chemotherapy within 1 week of craniotomy seemed to be less likely to have a recurrence than those who received chemotherapy more than 1 week after surgery. Thus, timing of perioperative chemotherapy may play a role in preventing late metastatic disease.
Selective angiographic embolization of the uterine arteries, instead of surgical intervention, may also be used to control uterine or pelvic tumor bleeding. In one case, after hydatidiform mole was diagnosed, hysterectomy was performed at first. Two years later, uterine artery embolization had to be performed because of active vaginal bleeding from the vaginal metastasis of the choriocarcinoma. Postoperative chemotherapy led to complete remission.
The limitation of this study is its retrospective nature. Selection bias might have been introduced because the surgical method was not randomized but determined by the surgeon. However, there were no drastic alterations of adjuvant surgical procedures, which may affect surgical outcomes in the management of GTN. One of the strengths of this study is the relatively large number of study subjects with GTN who received surgical treatment with consistency in its precision.
We conclude that adjuvant surgical procedures, especially hysterectomy and pulmonary resection for chemotherapy-resistant disease, as well as procedures to control hemorrhage, are pivotal in the management of GTN.
Fig. 1
A 16-week uterus filled with complete hydatidiform moles.
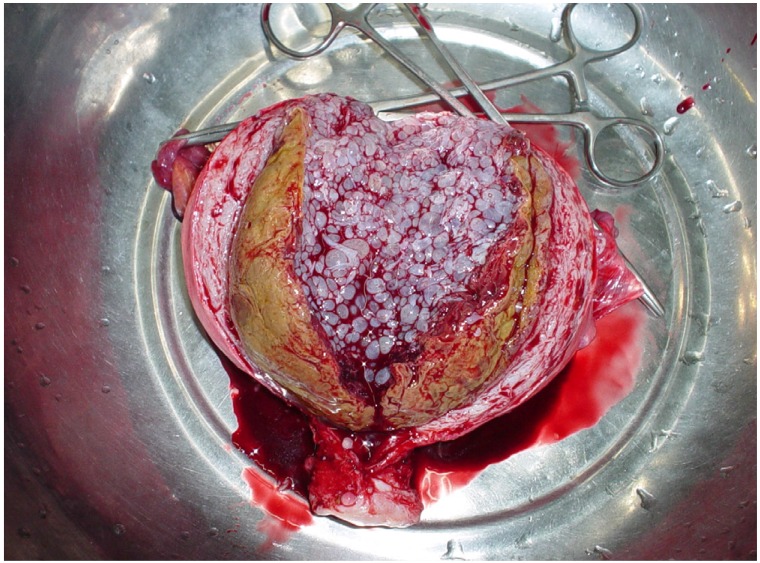
Table 1
Patient characteristics (n=32)
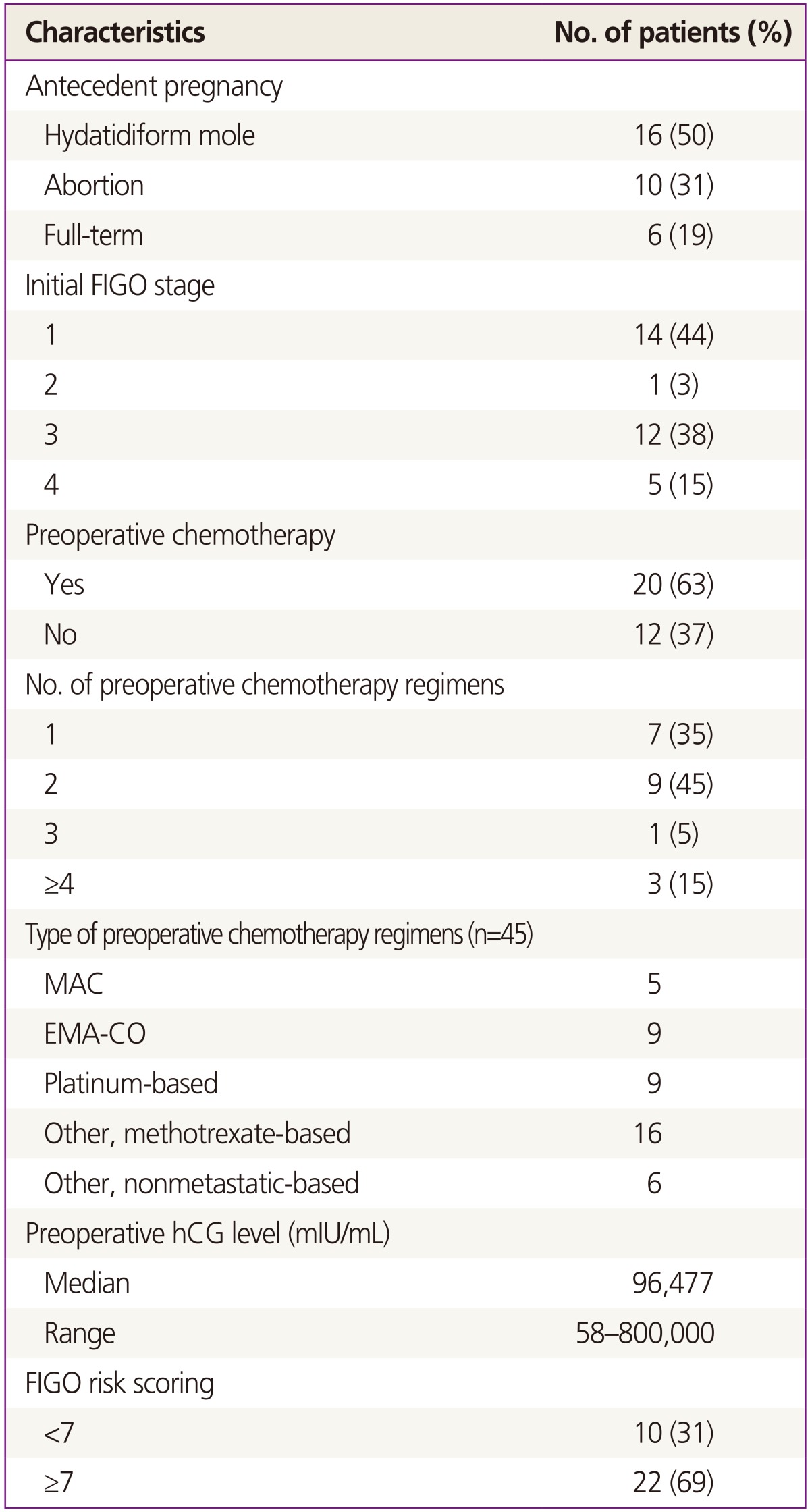
Table 2
Adjuvant surgical procedures and indication of surgery

Table 3
Salvage surgery for chemoresistant gestational trophoblastic neoplasia