Decreased bone mineral density is associated with coronary atherosclerosis in healthy postmenopausal women
Article information
Abstract
Objective
This study aimed to assess the association between bone mineral density (BMD) and coronary atherosclerosis in healthy postmenopausal women.
Methods
We performed a retrospective review of 252 postmenopausal women who had visited a health promotion center for a routine checkup. BMD of the lumbar spine (L1-L4) and femoral neck was evaluated using dual-energy X-ray absorptiometry, and coronary atherosclerosis was assessed using 64-row multidetector computed tomography. Participants were divided into normal BMD and osteopenia-osteoporosis groups, according to the T-scores of their lumbar spine or femoral neck.
Results
Participants with osteopenia-osteoporosis had a significantly higher proportion of coronary atherosclerosis than did those with normal BMD at the lumbar spine (P=0.003) and femoral neck (P=0.004). Osteopenia-osteoporosis at the lumbar spine (odds ratio [OR], 2.86; 95% confidence interval [CI], 1.12 to 7.27) or femoral neck (OR, 3.35; 95% CI, 1.07 to 10.57) was associated with coronary atherosclerosis, after controlling for age and cardiovascular risk factors.
Conclusion
Decreased BMD is associated with coronary atherosclerosis in healthy postmenopausal women, independent of age and cardiovascular risk factors. Postmenopausal women with decreased BMD may have a higher risk of developing coronary atherosclerosis.
Introduction
Coronary artery disease (CAD) is a major cause of death among postmenopausal women [1]. As time from the onset of menopause is closely related to the onset of coronary atherosclerosis, the prevalence of CAD has risen in tandem with increased life expectancy. As a result, the number of postmenopausal women who suffer from CAD is expected to increase over time. Therefore, identifying the risk factors associated with CAD in postmenopausal women is critical for reducing related mortality, along with associated healthcare costs.
Previous studies have demonstrated that osteoporosis and atherosclerosis have common etiological factors and mechanisms, suggesting that the presence of osteoporosis is a predictor of atherosclerosis [2,3,4]. According to recent studies, decreased bone mineral density (BMD) is associated with vascular calcification, which has been found to be a predictor of overall CAD incidence and mortality. Furthermore, several prospective studies have reported that low BMD and bone loss are risk factors for CAD-related mortality [5,6,7].
We have previously reported that values of brachial-ankle pulse wave velocity, an indicator of arterial stiffness, were significantly higher in an osteoporosis group (compared to osteopenia and normal BMD groups), and that these values were negatively associated with BMD [8]. These findings indicate that decreased BMD may increase the risk of developing coronary atherosclerosis. However, little is known about the association between decreased BMD and coronary atherosclerosis in postmenopausal woman; therefore, we chose to investigate the association between BMD and coronary atherosclerosis in healthy postmenopausal women.
Materials and methods
1. Participants
The study was approved by the institutional review board of Severance Hospital, Yonsei University College of Medicine. We performed a retrospective review of postmenopausal women who had visited the health promotion center at Gangnam Severance Hospital, Seoul, Korea for a routine checkup from March 2007 to December 2009. Body weight and height were measured in light indoor clothing, and body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). Blood pressure was assessed in the sitting position, after 10 minutes of rest, using an automated device (TM-2665P, A&D Co., Tokyo, Japan). All participants underwent dual-energy X-ray absorptiometry (DEXA) and 64-row multidetector computed tomography (64-MDCT) as part of the routine checkup.
We included postmenopausal women over 45-years-old, with menopause defined as 12 months of amenorrhea, subsequently confirmed by serum follicle-stimulating hormone levels >30 mIU/mL. Exclusion criteria included current smoking status, hypertension, diabetes mellitus, hypercholesterolemia, and cardiovascular disease. Participants who were receiving menopausal hormone therapy (MHT) or medication that might directly affect BMD were also excluded. A total of 252 participants who satisfied these criteria were included in the study analysis.
Physical activity was divided into two categories. Active exercise was defined as exercising three or more times per week for over 30 minutes. Alcohol intake was divided into two categories: those who consumed alcohol and those who did not.
2. Bone mineral density measurement
Areal BMD (g/cm2) was assessed using DEXA (QDR-Delphi; Hologic, Bedford, MA, USA) in the lumbar spine (L1-L4) and femoral neck. Participants were divided into normal BMD and osteopenia-osteoporosis groups, according to the T-scores of their lumbar spine and femur neck. Normal BMD, osteopenia, and osteoporosis were defined according to the World Health Organization's criteria. Osteoporosis was defined as bone density 2.5 or more standard deviations (SD) below the young adult mean (-2.5 SD or lower), and osteopenia was defined as bone density between 1 and 2.5 SD below the young adult mean (-1 to -2.5 SD) [9].
3. Coronary artery assessment
Cardiac computed tomography was performed using a 64-MDCT scanner (Philips Brilliance 64, Philips Medical System, Best, Netherlands). A β-blocker (40-80 mg of propranolol hydrochloride; Pranol, Dae Woong, Seoul, Korea) was administered orally 1 hour before the scan, to decrease the heart rate of women with a heart rate of ≥70 beats/min. Image reconstruction was performed on the scanner's workstation using commercially available software (Extended Brilliance Workstation, Philips Medical System). Coronary atherosclerosis was defined as any size of calcified, or non-calcified, atherosclerotic plaque with luminal narrowing.
4. Statistical analysis
Results were expressed as the mean±SD. The two-sample t-test was used to compare means of continuous variables, and the χ2-test was used to compare proportions of categorical variables. Logistic regression analysis was conducted to examine associations between decreased BMD and coronary atherosclerosis. Analyses were adjusted for age, alcohol intake, exercise, and vascular risk factors, which included BMI, fasting glucose levels, systolic blood pressure, and high-density lipoprotein (HDL) cholesterol levels.
All statistical analyses were conducted using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). A P-value less than 0.05 was considered to be of statistical significance.
Results
The average clinical and laboratory results for all participants are listed in Table 1. Age was significantly higher, and BMI was significantly lower, among women with osteopenia-osteoporosis compared to women with normal BMD. BMD values for the lumbar spine in the normal and osteopenia-osteoporosis groups were 1.01±0.09 and 0.85±0.10 g/cm2 respectively. BMD values for the femoral neck in the normal and osteopenia-osteoporosis groups were 0.77±0.06 and 0.62±0.07 g/cm2 respectively (Table 1).
Fig. 1 shows the proportion of coronary atherosclerosis in the normal BMD and osteopenia-osteoporosis groups. Participants with osteopenia-osteoporosis had a significantly higher proportion of coronary atherosclerosis at the lumbar spine (P=0.003) and femoral neck (P=0.004), when compared to those with normal BMD.
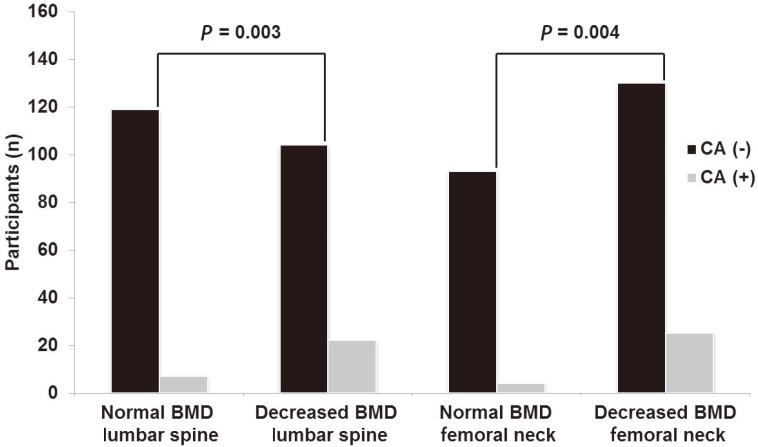
Distribution of CA (-) and CA (+) patients in normal and osteopenia-osteoporosis groups. CA, coronary atherosclerosis; BMD, bone mineral density.
Multiple regression analysis was performed to investigate the association between decreased BMD and coronary atherosclerosis. Osteopenia-osteoporosis at the lumbar spine (odds ratio [OR], 2.855; 95% confidence interval [CI], 1.121 to 7.23) and femoral neck (OR, 3.354; 95% CI, 1.065 to 10.569) was associated with coronary atherosclerosis, after controlling for age and vascular risk factors (Table 2).
Discussion
The present study revealed that decreased BMD was significantly associated with coronary atherosclerosis, independent of other risk factors. These findings suggest that postmenopausal women with decreased BMD may have a higher risk of developing coronary atherosclerosis. Our results confirmed a significant relationship between osteoporosis and coronary atherosclerosis, as previous studies have suggested, as well as a relationship between osteopenia and coronary atherosclerosis.
Menopause is a natural aging process, characterized by a decrease in estrogen and an increase in ferritin levels, during which a woman passes from her reproductive to non-reproductive years [10]. Estrogen deficiency impairs the normal bone remodeling cycle by increasing osteoclast resorption activity, without a corresponding increase in osteoblast activity, resulting in a net loss of bone [11]. Free iron deposits in tissues also create a pathological condition (iron overload), which impairs bone remodeling by inhibiting osteoblast proliferation and differentiation [12]. Meanwhile, it is well known that estrogen prevents the development of atherosclerosis, and that risk of CAD increases for postmenopausal women. In addition, excess iron in the tissues may catalyze the formation of highly reactive oxygen free radicals, which can trigger the development of atherosclerosis. Our previous study has shown that ferritin levels were associated with an increased risk of subclinical coronary atherosclerosis in postmenopausal women [13]. These facts suggest that decreased BMD may be associated with coronary atherosclerosis, especially in postmenopausal woman.
In postmenopausal women, osteoporosis and CAD are major causes of morbidity and mortality. Although MHT has been used to prevent these two diseases, MHT is no longer recommended as a first-line therapy for osteoporosis and CAD. Therefore, identification of individual with a high risk of the diseases is important for the prevention. As estrogen deficiency and iron overload in the postmenopausal period are common risk factors for both osteoporosis and CAD, measuring BMD may be a useful screening tool for identifying postmenopausal women with high-risk of developing osteoporotic fractures or CAD.
The key pathological step in atherosclerosis is thought to be the formation of calcified plaque on the endothelial surface. However, the results from previous studies are in disagreement regarding whether osteoporosis truly influences vascular calcification. In contrast to our results, some authors have indicated that there is no relationship between osteoporosis and atherosclerosis [14,15]. In another study, osteoporosis and coronary atherosclerosis were found to be independent processes in postmenopausal women, after adjusting for age, smoking status, diabetes mellitus, hypertension, and hypercholesterolemia [16]. However, other researchers have found that cardiovascular mortality is higher in women with low BMD [6]. Recent studies have also found that atherosclerotic calcification is associated with bone loss in postmenopausal women [17,18], and that a decrease in BMD may be related to subclinical atherosclerosis [7,19,20,21]. The mechanisms explaining the relationship between osteoporosis and CAD have not yet been elucidated, though it is believed that many other factors may be responsible; these factors have yet to be investigated.
We attempted to investigate the association between BMD and coronary atherosclerosis using 64-MDCT, which can accurately detect coronary atherosclerosis, even in asymptomatic individuals. Reported sensitivity and specificity of 64-MDCT range from 85% to 99% and 86% to 96%, respectively [22,23,24,25]. 64-MDCT has also improved the detection of non-calcified plaques, which, compared to calcified plaques, are considered more likely to be unstable and vulnerable to sudden rupture, subsequently increasing the risk of fatal ischemic cardiac events [26,27]. In another study, a considerable proportion of non-calcified plaques were found in asymptomatic low-risk patients with no, or mild, coronary calcium [28]. Moreover, we included only healthy postmenopausal women by excluding participants with a medical history of hypertension, diabetes mellitus, hypercholesterolemia, or cardiovascular disease. Therefore, correlation between BMD and CAD in previous studies and our study BMD is a considerable screening method for coronary atherosclerosis in healthy postmenopausal women, thereby facilitating early treatment and better outcomes.
Although our results are encouraging, the retrospective nature of the study precludes the possibility of investigating the causal relationship between bone loss and coronary atherosclerosis. In addition, our hospital-based design, and the limited number of participants, restricted our ability to reach a precise conclusion regarding the association between bone loss and coronary atherosclerosis. Larger longitudinal studies would likely be required to fully investigate the effects of bone loss on coronary atherosclerosis in postmenopausal women and clarify BMD is reliable screening method for CAD.
In conclusion, our results demonstrate that decreased BMD is associated with coronary atherosclerosis in healthy postmenopausal women, independent of age and cardiovascular risk factors. Therefore, postmenopausal women with low BMD may have a higher risk of developing coronary atherosclerosis.
Notes
No potential conflict of interest relevant to this article was reported.

