Mesenteric desmoid-type fibromatosis causing secondary hypertension in a young woman
Article information
Abstract
This report describes an 18-year-old woman presenting with abdominal distension, left flank pain, and hypertension. She had a huge abdominal mass, diagnosed as a mesenteric desmoid-type fibromatosis, causing compression of the left external iliac vessels and ureter, as well as elevated renin concentration and hypertension. After surgical removal of the mass, all signs improved including hypertension.
Introduction
Desmoid-type fibromatosis is a clonal fibroblastic proliferation characterized by infiltrative growth and an inability to metastasize [1]. This condition is unusual, with an estimated incidence of 2 to 4.3 new cases per million population per year [2,3,4]. Although histologically benign, they are locally aggressive with a propensity to compress local structures, such as the intestines, ureter, bladder, vagina, pelvic nerves, and major vessels [5]. We describe here a young woman with a pelvic fibromatosis causing secondary hypertension.
Case report
An 18-year-old woman was admitted in October 2012 with left flank pain and left leg swelling lasting one month. She also complained of abdominal distension with dysuria that had lasted for a few months. Her bowel function was normal and she had no recent weight loss. Her menstrual cycles were regular, she had no history of dysmenorrhea or dyspareunia, and she was sexually active. And she was not married yet. One year earlier, she had been diagnosed with hypertension but was not treated. There was no history of previous abdominal surgery or gynecologic disorders. Paternal hypertension was the only notable aspect of her family history.
At admission, her blood pressure was 160/100 mmHg, and other vital signs were stable. Physical examination showed that her abdomen was moderately distended. She had a tender mass in the central portion of abdomen but her gynecologic examination was normal. Complete blood screening profile and urinalysis were within normal limits. There was no elevation in serum tumor markers, including α-fetoprotein, β-human chorionic gonadotropin and CA-125. Her serum concentration of squamous cell carcinoma antigen had risen to 1.6 ng/mL, and C-reactive protein concentration to 2.7 mg/dL. Results of venereal disease research laboratory and treponema pallidum hemagglutination tests were positive, and renin concentration (activity) was 32.16 ng/mL/hr. Computed tomography (CT) scan showed a huge lobulated mass, about 17.2×15.6×13.5 cm in size, with heterogeneous attenuation, assumed to have occurred in left ovary (Fig. 1). Her uterus, right ovary, and bladder were deviated anterolaterally, and rectum was deviated to the right posterolateral side. Hydroure-teronephrosis due to obstructive uropathy and a large amount of fluid in the left renal subcapsule were evident. The mass also compressed her left external iliac vein.
An exploratory open laparotomy was performed. A low median skin incision was made with the patient in the supine position, revealing a huge pelvic mass partly covered with a thin fibrous capsule. No abnormalities were found in the uterus, both fallopian tubes and ovaries. The mass originated from the mesentery of the small bowel and was attached to the bowel and uterus. Adhesiolysis and extirpation of the mass were performed. Intraoperative frozen section histology of the mass was suspicious for a benign fibrotic tumor. The left retroperitoneum was opened, revealing a renal subcapsular cystic mass. The fluid in the cyst was drained.
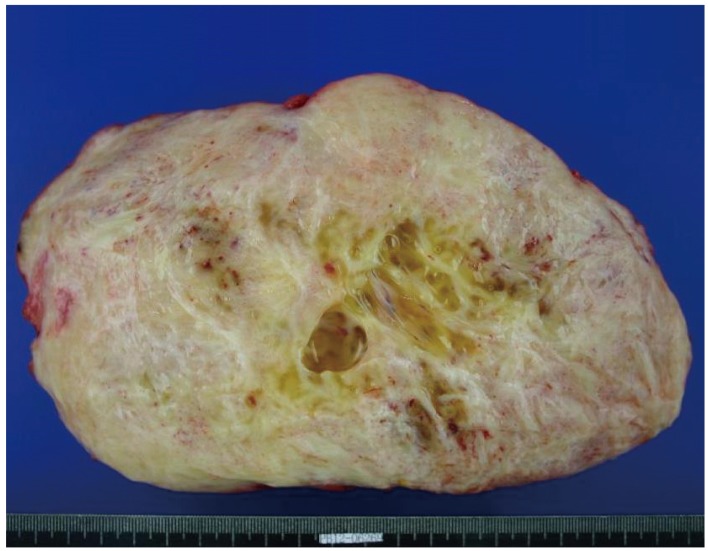
The specimen measured 21.5×14×13 cm and weighed 1,700 g. Microscopically, there was no evidence of ovarian or salpingeal tissue. A cut section revealed mainly solid parenchyma with myxofibrous cut surface. The central area showed cystic change with mucogelatinous content. Multifocal petechial hemorrhaging was noted, with no definite areas of parenchymal necrosis (Fig. 2). The tumor presented with a homogeneous appearance. Histological examination showed that the excised specimen was a desmoid-type fibromatosis with proliferation of fibroblasts in the collagenous stroma of the pelvic peritoneum. Cytologic examination of the left renal subcapsular cystic fluid revealed a pseudocyst or simple renal cortical cyst.
Following surgery, the patient was admitted to the intensive care unit for blood pressure monitoring. Over the next five days, her blood pressure normalized and renin level (activity) decreased to 1.57 ng/mL/hr. In addition, she was treated for early syphilis by intramuscular injection of benzathine penicillin G 2,400,000 units, although she had no symptoms of the disease. The patient was discharged on postoperative day 10 and was asymptomatic at her outpatient follow up visits one week and one month later.
Discussion
The etiology and natural history of abdominal fibromatoses remain unclear, but almost 75% of patients with abdominal fibromatosis have undergone previous abdominal surgery, suggesting that trauma may trigger the development of the fibromatosis [2,6,7]. In addition, mesenteric fibromatoses are common in patients with familial adenomatous polyposis, occurring in approximately 18% to 20% of such patients. Prolonged estrogen intake may also be involved in the formation of mesenteric fibromatoses in female patients of child-bearing age [2,7]. Nevertheless, these growths may occur spontaneously, in the absence of any predisposing factors and without association with other diseases, as with our patient. Fibromatosis with fibroblastic proliferation may therefore be the result of a defect in the regulation of normal cell growth, a defect that may be triggered by trauma or hormonal factors in some, but not all, patients.
Most intraabdominal fibromatoses affect the mesentery of the small bowel but can originate from any part of the peritoneal cavity, including the ileocolic ligament, mesocolon, and the root of the mesentery [2,3,4,8]. The mobility of the mesentery and the large potential space of the peritoneal cavity often permit an intraabdominal fibromatosis to develop into a huge mass before detection or to become inoperable due to extensive infiltrative spread. However, a mass weighing more than 1,700 g is rare, especially in young women.
The clinical presentation of an intraabdominal fibromatosis can vary greatly. Body weight loss, constipation, megaduodenum, urinary frequency, and nocturia have been reported [2,3,4,9,10]. The presentation in our patient, of secondary hypertension and elevated renin concentration, is much less common.
CT is useful in surgical planning and predicting the prognosis of mesenteric fibromatosis. Large tumor size (>10 cm), multiplicity, extensive tumor invasion, encasement of small bowel loops and entrapment of the ureter are factors associated with a poor prognosis in familial adenomatous polyposis patients with mesenteric fibromatosis [3,6]. Wide surgical excision is necessary when the mass is large or local structures are involved, as in our patient, but may result in significant morbidity, especially from a loss of the small intestine [11]. Patients with extensive infiltrative tumors may be treated nonsurgically, including with the estrogen receptor antagonist, tamoxifen; nonsteroidal anti-inflammatory agents; aromatase inhibitor therapy; chemotherapy with dactinomycin, vincristine, and cyclophosphamide; and/or radiotherapy [12,13,14]. Additional pharmacological treatments are being actively researched.
In conclusion, a huge pelvic mass has the possibility of various complications. Careful examination is required, even if the patient is very young.
Notes
No potential conflict of interest relevant to this article was reported.