 |
 |
- Search
| Obstet Gynecol Sci > Volume 60(2); 2017 > Article |
Abstract
Objective
The aim of this study was to determine recurrence factors and reproductive outcomes of laparoscopic myomectomy (LM) and minilaparotomic myomectomy (MM) for treating uterine leiomyomas.
Methods
Between 2007 and 2013, 160 patients underwent myomectomy, including 122 who underwent LM and 38 who underwent MM. Patients were followed up for recurrence based on pelvic ultrasound exams. Only patients who were followed up for a minimum of two years were selected for this retrospective study. Pregnancy rate, delivery, and delivery methods were compared between the two groups to evaluate reproductive outcomes. Furthermore, mean age, body mass index, preoperative administration of gonadotropin-releasing hormone agonist (GnRHa), and characteristics of leiomyomas were investigated to determine recurrence factors.
Results
The mean body mass index in the MM group was significantly (P=0.048) higher than that in the LM group. The number and the largest diameter of removed leiomyoma were also significantly higher in the MM group (both P=0.001). Logistic regression after adjusting significantly different characteristics showed that the LM group had shorter (P=0.020) postoperative hospitalization days compared to the MM group. Other outcome variables including recurrence rate were not significantly different between the two groups. Reproductive outcomes such as pregnancy rate, delivery, and delivery methods were not significantly different between the two groups. Preoperative GnRHa therapy was the only significant (P=0.039) recurrence factor after myomectomy.
Uterine leiomyoma is the most common uterine neoplasm. It is diagnosed in about 25% to 30% of women [1]. Open myomectomy is a conservative treatment primarily used for symptomatic leiomyomas. However, laparoscopic myomectomy (LM) has become a more attractive option because it is less invasive, producing less postoperative pain with shorter recovery time compared to open myomectomy [2,3]. Nevertheless, LM can be a difficult procedure since it takes longer time to be skilled with technical difficulties for treating large and multiple leiomyomas.
Minilaparotomic myomectomy (MM), an alternative to LM, has been considered as a valid and cost-effective treatment [4]. A recent study has reported that laparoscopic surgery represents a truly minimally invasive surgical approach that can be used safely for the management of benign and neoplastic gynecologic diseases [5,6,7]. Although several studies have compared the surgical and reproductive outcomes of laparotomy to those of LM [8,9], few long-term data are available on the effectiveness and morbidity of laparoscopic and minilaparotomic approaches for treating uterine leiomyomas. Only one randomized controlled trial compared the short-term outcomes of LM and MM and demonstrated that both procedures are safe and minimally invasive. However, the study did not focus on the difference in recurrence or future fertility between the two groups [10]. Therefore, the purpose of this study was to determine recurrence factors and reproductive outcomes of LM and MM for treating uterine leiomyomas.
A total of 160 women who underwent surgery with either LM or MM at Chungnam National University Hospital were enrolled in this study from October 2007 to May 2013. This study was approved by the institutional review board of the hospital and the requirement for informed consent was waived due to its retrospective nature (2016-04-011). Detailed history data including demographic characteristics, menstrual, obstetric, medical, and surgical history, fertility, and pregnancy outcomes were obtained from medical records. In this study, all patients were operated on by one surgeon and followed up for more than 2 years.
Indications for myomectomy were unexplained infertility or leiomyoma-related symptoms. Leiomyomas were subserosal or intramural type. Their sizes ranged from 3 to 10 cm and their numbers ranged from 1 to 10. Symptoms mainly comprised of the following: urinary retention, voiding difficulty or frequency, secondary dysmenorrhea, low back pain, and severe anemia from heavy menstrual bleeding.
Preoperative work-up consisted of pelvic exams and pelvic ultrasounds to establish the volume and consistency of the uterus as well as the number, size, locations, and types of leiomyomas. Magnetic resonance imaging was performed when the exact nature of the leiomyomas could not be determined by ultrasound. After preoperative work-up, gonadotropin-releasing hormone agonist (GnRHa) was injected 2 to 3 times at a monthly interval to patients with anemia or leiomyomas of larger than 8 cm in diameter. For postoperative follow up, pelvic ultrasound exams were conducted at 1 month after the operation to check residual leiomyomas. Afterwards, routine pelvic ultrasound exams were conducted every 6 to 12 months.
Of the 160 patients, 122 underwent LM and 38 women underwent MM. The surgeon involved was skilled in both procedures. First, the decision to perform LM or MM was made preoperatively based on the characteristics of the patient and leiomyomas. Next, we observed and confirmed the location of the lesion and the size and shape of the uterus with a laparoscope. After that, the final decision on the type of surgical method was made. In our study, MM was performed on principle when the size of leiomyoma was larger than 8 cm or its number was more than three. However, in rare cases, LM was performed when the type of leiomyomas was intraligamental or pedunculated even if it satisfied the criteria for MM mentioned above. There was no case report of conversion from LM to MM during surgery in this study. We excluded patients who had submucosal leiomyomas, adnexal abnormalities at ultrasound and residual leiomyomas detected at 1 month by postoperative ultrasound examination in present study. Recurrence was defined as a reappearance of leiomyomas on clinical examination and leiomyomas of more than 2 cm in diameter on ultrasound.
The distributions of patient characteristics between LM and MM were compared to each other using two-sample t-test for continuous variables and chi-square test (or Fisher's exact test when the expected frequency within any cell was <5) for categorical variables. Multivariate logistic regression analysis was used to determine the adjusted odds ratios of the MM group. Variables considered as potential confounders in multivariate analysis were body mass index (BMI), the mean number of leiomyomas, and the mean diameter of the largest leiomyoma. Cumulative event (recurrence) rate was calculated with the Kaplan-Meier method using the time to the first event as outcome variable. The differences between the two groups were tested with log-rank test. In addition, Cox proportional hazards model was used to calculate the hazard rate for recurrence after myomectomy. A P-value of less than 0.05 was considered as statistically significant. Statistical analysis was performed with the SPSS ver. 18 (SPSS Inc., Chicago, IL, USA).
The demographic and clinical characteristics of the LM and MM groups are summarized in Table 1. The mean age and parity of patients in the LM and MM group were similar to each other (age, 33.9±5.4 vs. 35.2±4.9 years, P=0.192; parity, 0.5±0.9 vs. 0.4±0.8, P=0.507). Indication of myomectomy, type and localization of leiomyomas, history of previous abdominal operation, and preoperative administration of GnRHa were also similar between the two groups. The mean BMI was significantly higher in the MM group than that in the LM group (23.9±4.9 vs. 22.1±2.7 kg/m2, P=0.048). The mean number of removed leiomyoma (6.2±1.3 vs. 2.2±1.3, P=0.001) and the diameter of the largest leiomyoma (8.3±2.0 vs. 4.6±2.2, P=0.001) were significantly higher in the MM group compared to those in the LM group.
The mean blood loss and surgical time were significantly higher in the MM group than those in the LM group (blood loss, 228±44 vs. 140±34 mL, P=0.044; surgical time, 110±6.3 vs. 80±5.9 minutes, P=0.001). In addition, the length of postoperative hospitalization days was significantly longer in the MM group than that in the LM group (6.7±0.3 vs. 5.5±0.2 days, P=0.001). However, there was no significant difference in postoperative complication rates such as fever and ileus between the two groups. Recurrence rate was also similar to each other between the two groups (17% [21 of 122 patients] in the LM group and 21% [8 of 38 patients] in the MM group, P=0.632). There was no re-hospitalization within 30 days of surgery in LM or MM group. Reproductive outcome was also similar in the two groups. Live birth rates were 29% (23 of 80 patients) in the LM group and 48% (12 of 25 patients) in the MM group (P=0.076). Time to first pregnancy, delivery, and delivery methods were also similar to each other between the two groups.
The calculations above were later adjusted using logistic regression in an effort to control several variables that might affect the results. Before using the logistic regression model, BMI, size, and numbers of leiomyomas were very different in the two groups. However, they were controlled with the adjustment. We adjusted the odds ratios of the MM over LM group and calculated each P-value (Table 2). Postoperative hospitalization stay (P=0.020) was the only variable that showed significance. All other surgical and reproductive outcomes were not significantly different between the two groups. Especially, the recurrence rate did not differ between the two groups (P=0.244)
The median follow-up time for all patients was 40 months (range, 24 to 109 months) and the median time from myomectomy to recurrence was 31 months (range, 6 to 44 months). Recurrence was analyzed with clinical factors that might have affected recurrence. Of all variables, only preoperative administration of GnRHa showed significant association with recurrence (P=0.039) (Table 3). All other clinical factors and comparison between the two surgical methods of myomectomy did not show significance. Therefore, multivariate analysis was not performed. Kaplan-Meier curve in Fig. 1 showed significant difference in recurrence for preoperative administration of GnRHa.
In this study, LM and MM were not significantly different in most surgical outcomes including the recurrence rate. Nonetheless, we found significant difference in postoperative hospitalization stay between the two groups. Alessandri et al. [10] have also compared LM and MM with a randomized controlled study and reported that LM groups requires less postoperative analgesics and recovers faster postoperatively. In terms of reproductive outcomes, we found no significant difference between MM and LM concerning cumulative live birth rate, time to first pregnancy, or delivery. Consistent with our results, Malzoni et al. [11] have reported that both LM and MM can improve reproductive outcomes to similar extents in patients with unexplained infertility. Therefore, surgical method is not an important determinant of postoperative pregnancy rates. However, further prospective randomized control studies are needed to confirm these results.
In addition to surgical and reproductive outcomes, we focused on factors that might affect recurrence. Factors affecting recurrence in myomectomy have been studied previously [12,13,14]. According to Radosa et al. [12], patients in the third decade of life and diagnosed with more than one leiomyoma have increased risk of recurrence. In our study, preoperative administration of GnRHa was the only factor that significantly affected recurrence. Preoperative administration of GnRHa was used to decrease the size of leiomyomas prior to surgery. This result indicating that preoperative administration GnRHa might prevent the identification of small leiomyomas.
In our study, patients' characteristics, diameter of the largest leiomyoma, number of leiomyomas, and mean BMI were significantly different between the two groups. Marret et al. [15] have reported that the diameters and numbers of leiomyomas are significantly higher in abdominal myomectomy group than those in LM group. According to Sparic et al. [16], obesity do not have consistent association with the risk of leiomyomas. However, some articles claim that obesity can increase the risk of leiomyomas [17,18,19]. In this study, the mean BMI was higher in the MM group than that in the LM group. Since the MM group had larger sizes or more numbers of leiomyomas, there might be a correlation between obesity and leiomyomas. However, obesity was not considered as a variable when we selected the operation method in our study.
With respect to study limitations, there are largely three impediments that warrant attention. First, given that the study design was retrospective, the possibility of missing data was unavoidable. For instance, we only included patients with a follow-up of >2 years. This not only reduced the quality of the database, but also generated selection bias. Second, the accuracy of examination is questionable. Magnetic resonance imaging scans are more accurate than ultrasounds in screening uterine leiomyomas. However, due to the expense of examination, we used ultrasounds for identification of uterine leiomyomas instead of magnetic resonance imaging. Lastly, a potential limitation can arise from the annual ultrasounds in this study. Such use has enabled us to detect recurred leiomyomas. However, consequently there might be a tendency of overestimating recurrence rates. This might explain the discrepancy between our study and previous studies in which ultrasounds were only conducted in the presence of symptoms. Despite these limitations, this study has its merit in that it is the first study that compares the recurrence and reproductive outcome between LM and MM. In addition, our study was able to minimize the gap in the outcomes among different operators because only one surgeon performed both LM and MM.
In conclusion, this study shows that LM and MM are two surgical methods that have similar recurrence rates and reproductive outcomes. The only recurrence factor of significance was pre-operative administration of GnRHa. However, randomized prospective control study is needed to confirm the results of this study.
References
1. Marshall LM, Spiegelman D, Barbieri RL, Goldman MB, Manson JE, Colditz GA, et al. Variation in the incidence of uterine leiomyoma among premenopausal women by age and race. Obstet Gynecol 1997;90:967-973. PMID: 9397113.


2. Jin C, Hu Y, Chen XC, Zheng FY, Lin F, Zhou K, et al. Laparoscopic versus open myomectomy: a meta-analysis of randomized controlled trials. Eur J Obstet Gynecol Reprod Biol 2009;145:14-21. PMID: 19398260.


3. Kaminski P, Gajewska M, Wielgos M, Sodowski K, Szymusik I, Bartkowiak R, et al. Laparoscopic treatment of uterine myomas in women of reproductive age. Neuro Endocrinol Lett 2008;29:163-167. PMID: 18283255.

4. Benedetti-Panici P, Maneschi F, Cutillo G, Scambia G, Congiu M, Mancuso S. Surgery by minilaparotomy in benign gynecologic disease. Obstet Gynecol 1996;87:456-459. PMID: 8598975.


5. Fagotti A, Ferrandina G, Longo R, Mancuso S, Scambia G. Minilaparotomy in early stage endometrial cancer: an alternative to standard and laparoscopic treatment. Gynecol Oncol 2002;86:177-183. PMID: 12144825.


6. Fanfani F, Fagotti A, Ercoli A, Bifulco G, Longo R, Mancuso S, et al. A prospective randomized study of laparoscopy and minilaparotomy in the management of benign adnexal masses. Hum Reprod 2004;19:2367-2371. PMID: 15242993.


7. Fanfani F, Fagotti A, Longo R, Marana E, Mancuso S, Scambia G. Minilaparotomy in the management of benign gynecologic disease. Eur J Obstet Gynecol Reprod Biol 2005;119:232-236. PMID: 15808386.


8. Mais V, Ajossa S, Guerriero S, Mascia M, Solla E, Melis GB. Laparoscopic versus abdominal myomectomy: a prospective, randomized trial to evaluate benefits in early outcome. Am J Obstet Gynecol 1996;174:654-658. PMID: 8623802.


9. Seracchioli R, Rossi S, Govoni F, Rossi E, Venturoli S, Bulletti C, et al. Fertility and obstetric outcome after laparoscopic myomectomy of large myomata: a randomized comparison with abdominal myomectomy. Hum Reprod 2000;15:2663-2668. PMID: 11098042.


10. Alessandri F, Lijoi D, Mistrangelo E, Ferrero S, Ragni N. Randomized study of laparoscopic versus minilaparotomic myomectomy for uterine myomas. J Minim Invasive Gynecol 2006;13:92-97. PMID: 16527709.


11. Malzoni M, Tinelli R, Cosentino F, Iuzzolino D, Surico D, Reich H. Laparoscopy versus minilaparotomy in women with symptomatic uterine myomas: short-term and fertility results. Fertil Steril 2010;93:2368-2373. PMID: 19285666.


12. Radosa MP, Owsianowski Z, Mothes A, Weisheit A, Vorwergk J, Asskaryar FA, et al. Long-term risk of fibroid recurrence after laparoscopic myomectomy. Eur J Obstet Gynecol Reprod Biol 2014;180:35-39. PMID: 25016181.


13. Yoo EH, Lee PI, Huh CY, Kim DH, Lee BS, Lee JK, et al. Predictors of leiomyoma recurrence after laparoscopic myomectomy. J Minim Invasive Gynecol 2007;14:690-697. PMID: 17980328.


14. Doridot V, Dubuisson JB, Chapron C, Fauconnier A, Babaki-Fard K. Recurrence of leiomyomata after laparoscopic myomectomy. J Am Assoc Gynecol Laparosc 2001;8:495-500. PMID: 11677326.


15. Marret H, Chevillot M, Giraudeau B. Study Group of the French Society of Gynaecology and Obstetrics (Ouest Division). A retrospective multicentre study comparing myomectomy by laparoscopy and laparotomy in current surgical practice What are the best patient selection criteria? Eur J Obstet Gynecol Reprod Biol 2004;117:82-86. PMID: 15474250.


16. Sparic R, Mirkovic L, Malvasi A, Tinelli A. Epidemiology of uterine myomas: a review. Int J Fertil Steril 2016;9:424-435. PMID: 26985330.

17. Sommer EM, Balkwill A, Reeves G, Green J, Beral DV, Coffey K, et al. Effects of obesity and hormone therapy on surgically-confirmed fibroids in postmenopausal women. Eur J Epidemiol 2015;30:493-499. PMID: 25784364.



18. Pandey S, Bhattacharya S. Impact of obesity on gynecology. Womens Health (Lond) 2010;6:107-117. PMID: 20088734.


19. Takeda T, Sakata M, Isobe A, Miyake A, Nishimoto F, Ota Y, et al. Relationship between metabolic syndrome and uterine leiomyomas: a case-control study. Gynecol Obstet Invest 2008;66:14-17. PMID: 18230910.


Fig. 1
Cumulative recurrence of leiomyomas with and without preoperative administration of gonadotropin-releasing hormone (GnRH) agonist with Kaplan-Meier curve.
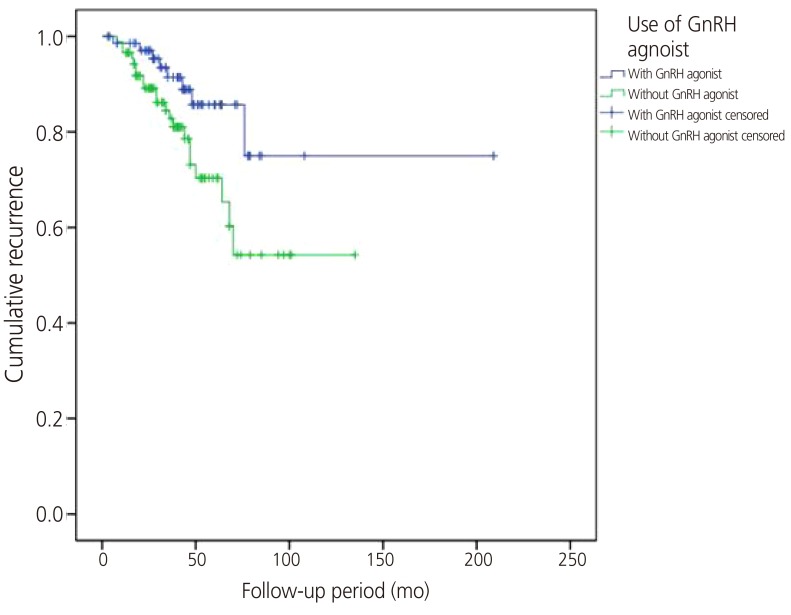
Table 1
Comparison of patient's characteristics between laparoscopic myomectomy and minilaparotomic myomectomy group
Table 2
Logistic regression analysis for surgical and reproductive outcome
Table 3
Univariate analysis of recurrence after myomectomy
-
METRICS

- Related articles in Obstet Gynecol Sci
-
Comparsion of Laparoscopic with minilaparotomic myomectomy in uterine myoma.2002 March;45(3)




















