|
 |
- Search
| Obstet Gynecol Sci > Volume 58(3); 2015 > Article |
Abstract
Objective
This study aimed to examine clinical practice patterns in the management of pregnant women admitted with threatened preterm labor (TPL) in Korea.
Methods
Data from women admitted with a diagnosis of TPL were collected from 22 hospitals. TPL was defined as regular uterine contractions with or without other symptoms such as pelvic pressure, backache, increased vaginal discharge, menstrual-like cramps, bleeding/show and cervical changes. Data on general patient information, clinical characteristics at admission, use of tocolytics, antibiotics, and corticosteroids, and pregnancy outcomes were collected using an online data collections system.
Results
A total of 947 women with TPL were enrolled. First-line tocolysis was administered to 822 (86.8%) patients. As a first-line tocolysis, beta-agonists were used most frequently (510/822, 62.0%), followed by magnesium sulfate (183/822, 22.3%), calcium channel blockers (91/822, 11.1%), and atosiban (38/822, 4.6%). Of the 822 women with first-line tocolysis, second-line tocolysis were required in 364 (44.3%). Of 364 with second-line, 199 had third-line tocolysis (37.4%). Antibiotics were administered to 29.9% of patients (284/947) with single (215, 22.7%), dual (26, 2.7%), and triple combinations (43, 4.5%). Corticosteroids were administered to 420 (44.4%) patients. Betamethasone was administered to 298 patients (71.0%), and dexamethasone was administered to 122 patients (29.0%).
Threatened preterm labor (TPL) is the progression of cervical dilatation and ripening caused by regular uterine contractions occurring before 37 weeks of pregnancy, which may result in preterm birth. Preterm birth, the most common cause of neonatal mortality and morbidity worldwide [1,2], causes over 70% of fetal death rates and approximately 50% of neonatal neural deficits [3,4,5]. Preterm birth occurs in 5 to 18% of pregnancies, and is also a common cause of hospitalization during the antenatal period [6,7,8]. With the aim of prolonging gestation, improving neonatal outcomes, and reducing the burden of maternal and fetal complications, various approaches to the management of preterm labor have been extensively investigated [9]. However, solid evidence regarding the effectiveness of these approaches is still lacking, as some drugs have reportedly shown adverse effects. With the exception of some defined recommendations, i.e., single course of corticosteroids and tocolytic treatment up to 48 hours, clinical practice patterns for TPL vary considerably between countries [10].
Although TPL treatment in Korea includes the use of tocolytics, antibiotics, and steroids, studies or surveys aimed at establishing treatment guidelines for the clinical management of TPL have been quite lacking until now. As the management of TPL differs from individual to individual, and from hospital to hospital, this study aimed to examine clinical practice patterns in the management of women with TPL in Korea.
Pregnant women admitted to 22 hospitals with a diagnosis of TPL from January 1 to December 31, 2012 were enrolled in this study. Inclusion criteria at admission included women from 24+0 to 33+6 weeks' gestation with singleton or twin pregnancies and diagnosis of TPL. TPL was defined as regular uterine contractions with or without other symptoms such as pelvic pressure, backache, increased vaginal discharge, menstrual-like cramps, bleeding/show and cervical changes [11,12,13]. Women with preterm premature rupture of membranes (PPROM), cervical insufficiency, triplet and higher-order multifetal pregnancy, diabetes, renal disease, pregnancy associated hypertension, chronic hypertension, cardiovascular illness, symptomatic infectious diseases, chronic medical disorders, and those with a fetal structural or genetic anomaly were excluded from the study. The study protocol was developed and supervised by the Preterm Birth Research Group affiliated to the Korean Society of Maternal Fetal Medicine. Data were obtained using an online data collection system available at the following website: http://fetalmed.or.kr/bbs/?code=preterm. Participants responded to multiple-choice or yes/no questions by clicking the appropriate button, and added numeric data values directly into blank boxes. Data on general patient information, clinical characteristics of the subjects at admission, tocolytics, antibiotics, and steroids use during hospitalization were collected retrospectively. The institutional review board approved this study (KUH1040027).
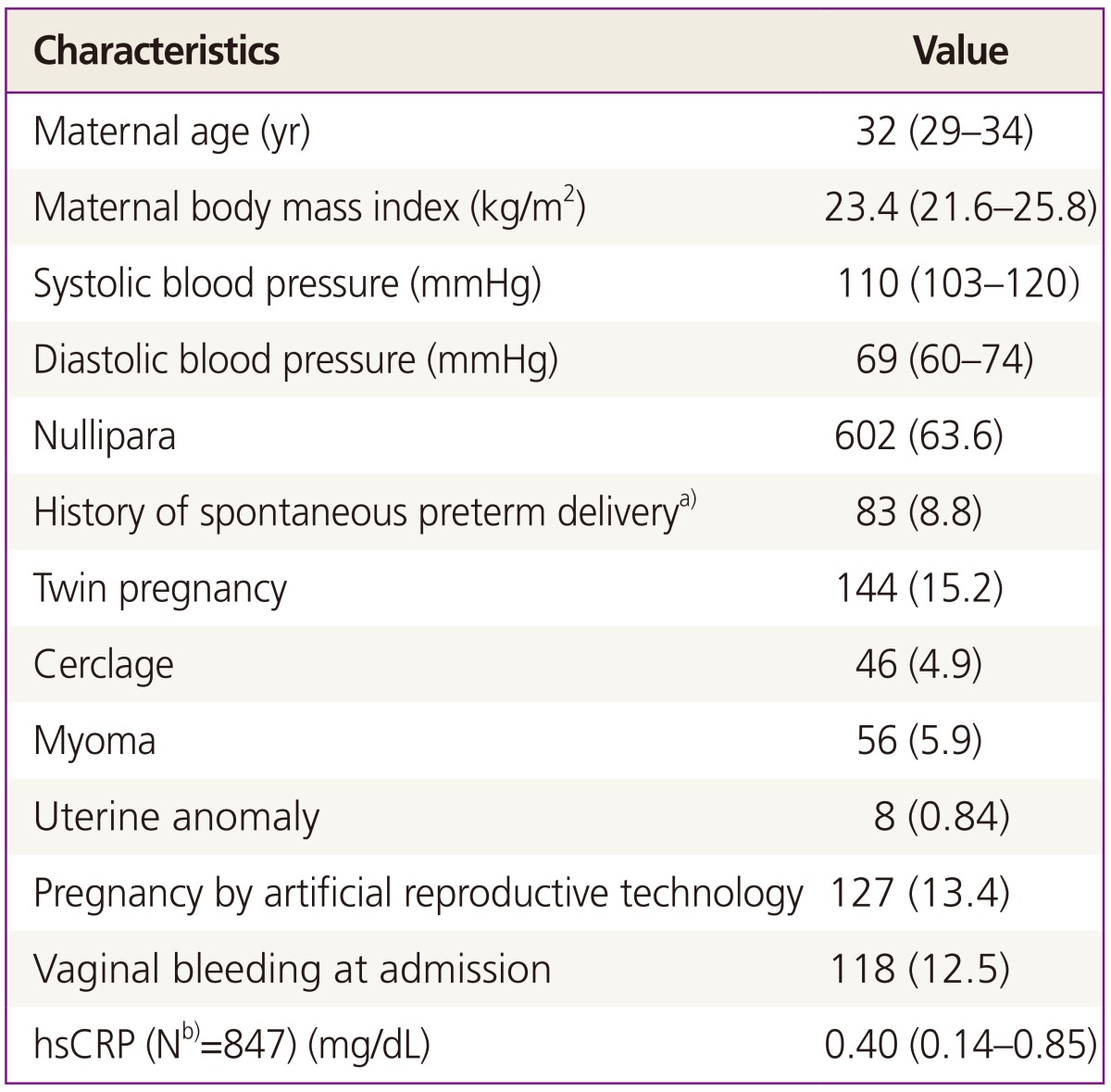
Basic information was collected according to the diagnosis given at admission. Clinical and obstetric characteristics of the patients were obtained which include maternal age, body mass index, blood pressure, parity, history of spontaneous preterm delivery, twin pregnancy, history of cerclage, myoma, uterine anomaly, pregnancy achieved through artificial reproductive technology, vaginal bleeding at admission.
Tocolytic therapy including beta-agonists, magnesium sulfate, atosiban, and calcium channel blockers was administered using a first-line to third-line drug approach. Women who received other rarely administered or a combination of two or more tocolytics were excluded from the study. First-line tocolysis was defined as tocolytic drug treatment firstly administered at admission, regardless of route of administration. Second- and third-line tocolysis were defined as treatment with an alternative tocolytic drug after the previous tocolysis treatment failed. Causes of tocolytic treatment failure leading to the unintended discontinuation of tocolytic treatment included side effects, poor tolerance, and insufficient efficacy. Although all women with TPL should not be treated with antibiotics, antibiotics in women with TPL can be used in cases of group B streptococcal infection, cervical infection, chorioamnionitis, etc. The antibiotic treatment patterns were investigated using the following variables: antibiotic treatment, frequency and duration of treatment, type of antibiotics, and type of regimen i.e., single, double or triple combination therapy. We also investigated the use of the antenatal corticosteroids. Two different regimens were used, which include four doses of 5 mg dexamethasone intramuscular injections every 12 hours and two doses of 12 mg betamethasone intramuscular injections every 24 hours [14]. Patients who received two or more courses of corticosteroid therapy were excluded.
In women who delivered at term and in the participating hospitals, pregnancy outcomes were collected which included gestational age at delivery, mode of delivery, presence or absence of histologic chorioamnionitis.
Birth weight, one minute and five minutes Apgar score, and admission to neonatal intensive care unit (NICU) were investigated as neonatal outcomes.
A total of 947 pregnant women with a diagnosis of TPL were enrolled in this study. The frequency of admissions was increased in proportion to the number of gestational weeks (Fig. 1). Clinical and obstetric characteristics in women with TPL are shown in Table 1. Nulliparous women comprised 63.6% of the total, and 83 (8.8%) had a history of spontaneous preterm delivery.
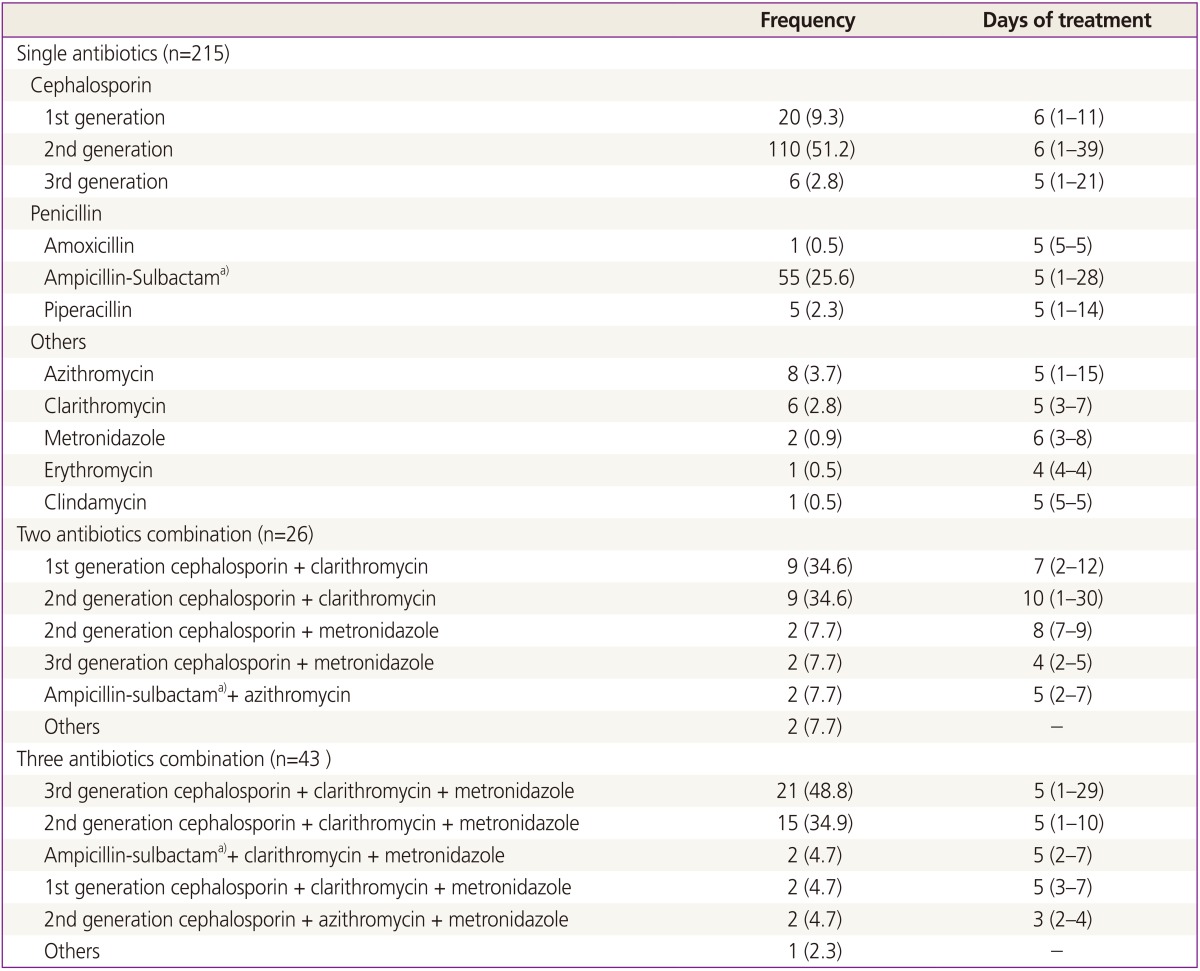
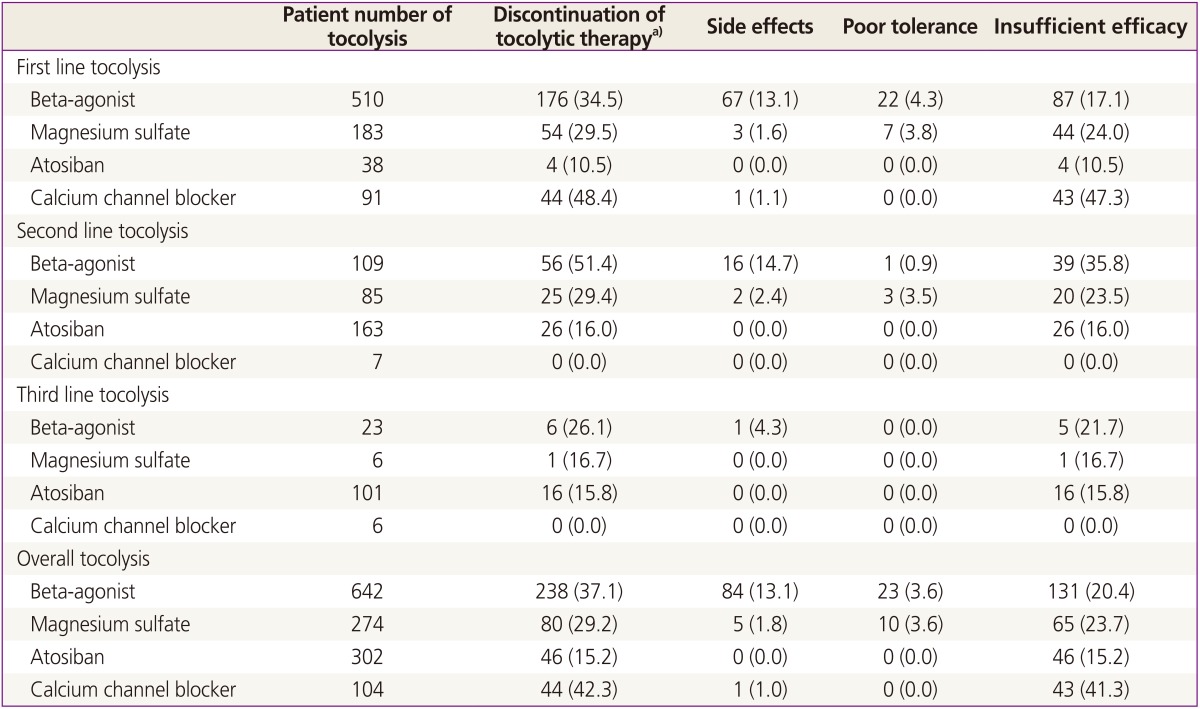
The practice pattern of tocolytic therapy is summarized in Table 2. Among 947 women hospitalized for TPL, first-line tocolysis was administered to 822 (86.8%) women. Beta-agonists were the most frequently used agents (510/822, 62.0%), followed by magnesium sulfate (183/822, 22.3%), calcium channel blockers (91/822, 11.1%), and atosiban (38/822, 4.6%). Of the 822 women receiving first-line tocolytic treatment, 364 (44.3%) required a second-line drug. Similarly, women who received a second-line drug were switched to third-line tocolytic treatment (136/364, 37.4%). Side effects were most frequently found in beta-agonists (84/642, 13.1%) including maternal tachycardia, chest discomfort, dyspnea, tremor, pleural effusion, pulmonary edema, dizziness, uncontrolled blood glucose, tingling sensation in extremities, and elevated liver enzymes. Among the tocolytic agents, calcium channel blockers showed the most insufficient efficacy (43/104, 41.3%). Antibiotics were administered to 284 women (284/947, 29.9%), with single (215, 22.7%), dual (26, 2.7%), and triple antibiotic combination therapy (43, 4.5%) (Table 3). The single antibiotic most frequently administered was 2nd generation cephalosporin only with a median treatment duration of 6 days. Among the triple antibiotic therapies, the combination of a 3rd generation cephalosporin + clarithromycin + metronidazole was the most frequently used. Among women who received antenatal corticosteroid therapy (420/947, 44.4%) for fetal lung maturation, 298 (71.0%) and 122 (29.0%) received betamethasone and dexamethasone, respectively (Fig. 2). The completion rate of a course of corticosteroid therapy was higher in women receiving betamethasone than in those receiving dexamethasone.
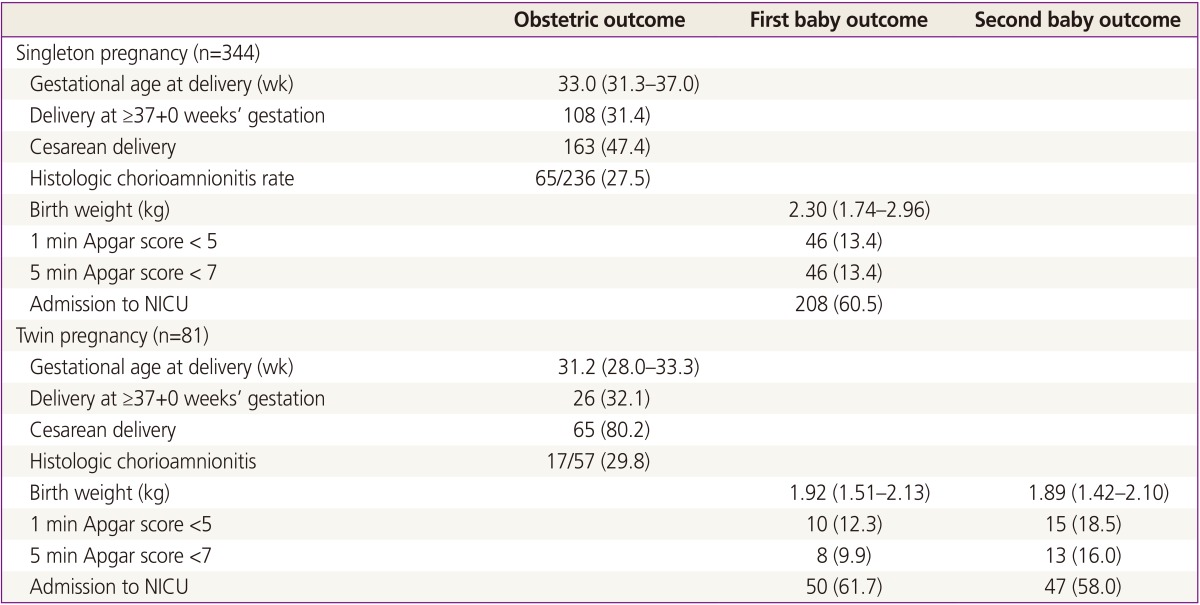
Of 947 pregnant women with TPL initially enrolled in this study, 425 (44.9%), including 344 and 81 women with singleton and twin pregnancies, respectively, were followed up until delivery. Table 4 shows pregnancy outcomes of the 425 pregnant women
with complete follow up.
The term TPL is more often used in the clinical and investigational fields. However, as the definition of TPL is not yet well established, there is considerable variability between studies. The mechanism of preterm labor is not clear, thereby hindering the development of successful preventive methods and making large practice variation for treatment of TPL. TPL has been defined as the presence of at least 3 regular and painful uterine contractions within a 30-minute period [15], or the presence of at least two uterine contractions every 10 min for 60 minutes, in combination with cervical changes ascertained on digital examination, and/or cervical length <30 mm measured by transvaginal ultrasonography [16]. Others have defined TPL as the occurrence of persistent premature uterine contractions between 20 and 37 weeks of gestation accompanied by other symptoms such as pelvic pressure, backache, increased vaginal discharge, menstrual-like cramps, bleeding/show and shortened cervix [17]. True preterm labor is known to involve regular painful uterine contractions accompanied by cervical changes. However, other clinical manifestations such as vaginal bleeding, mild or irregular contraction, menstrual-like cramping, PPROM, and short cervix that may overlap with true preterm labor, can hamper the clinical discrimination between true preterm labor and TPL. It is not easy to discriminate true preterm labor from TPL in clinical field. As most women presenting with TPL are at an increased the risk of preterm birth, they are usually admitted. Thus, pregnant women with TPL were enrolled in this study, though they might not have true preterm labor.
Present treatments in TPL focus on the inhibition of preterm uterine contractions, at the end point of the cascade of the pathophysiological process. The treatment of women at risk of preterm delivery consists of administration of tocolytic drugs for 48 hours to allow for administration of corticosteroids and transportation of the patient to a center with NICU facilities in case if gestational age is <32 weeks [18]. Beta-agonists were the most frequently used tocolytics. Side effects occurred most frequently in women treated with beta-agonists (13.1%). This study provided an overview of the current insight in tocolysis in TPL in Korea.
Recent study showed that there was no demonstrable benefit in important neonatal outcomes with prophylactically or routinely giving antibiotics to women in preterm labor with intact membranes in the absence of overt signs of infection [19]. It is unknown that in utero exposure of various antibiotics is safe on the preterm neonate. Nevertheless, the patterns of antibiotics use for TPL were quiet variable, and treatment duration was about 5 to 6 days in Korea. Based on this study, the rate of antibiotics use was very high in preterm labor with intact membranes. It is needed that the antibiotics use is restricted to specific cases such as chorioamnionitis, cervical infection.
Although dexamethasone may have some benefits compared with betamethasone such as less intraventricular hemorrhage, and a shorter length of stay in the NICU, it remains unclear whether one corticosteroid has advantages over another, and there are no available long-term results [14]. In this study, betamethasone is more frequently used and higher completion rate than dexamethasone in Korea. This discrepancy may be explained by a higher tolerability of the betamethasone regimen, as a total of two doses were administered intramuscularly every 24 hours, compared with four dexamethasone doses administered intramuscularly every 12 hours.
This retrospective study had several limitations. First, because medical records differed between institutions, the collection of uniformed patient data was difficult. Second, the criteria for admission and treatment in pregnant women with TPL also differed between hospitals. For example, pregnant women who had regular uterine contractions alone without cervical changes were hospitalized in some institutions, but in others, women with both, regular uterine contractions and cervical changes were admitted. Some hospitals administered single antibiotics routinely, whereas others administered dual and triple antibiotic combinations. Third, because of a lack of NICU beds, maternal medical problems, or fetal congenital anomalies, a considerable number of women with TPL experienced one or more hospital-to-hospital transfers, which may have resulted in losses to follow up, and difficulties in the collection of serial medical data. Fourth, the diagnostic criteria of neonatal morbidity such as respiratory distress syndrome, bronchopulmonary dysplasia, necrotizing enterocolitis, and retinopathy of prematurity were also different between institutions. Fifth, in this study, the data for the maintenance therapy after initial tocolysis and the use of magnesium sulfate for neuroprotection effect were not collected. Further study for these treatments will be studied in the near future.
The results of this retrospective multicenter study have provided baseline data on practice patterns for TPL. However, further efforts are needed in order to develop a standardized registration system for women with TPL, in which pregnancy and neonatal outcome data are linked to nationwide neonatology and preventive medicine multicenter registries. The data generated from these interconnected systems will provide powerful information to ultimately improve pregnancy and neonatal outcomes, as well as facilitate the development of standardized practice guidelines for TPL management in Korea.
Acknowledgments
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant no. HI14C0306).
References
1. Meloni A, Melis M, Alba E, Deiana S, Atzei A, Paoletti AM, et al. Medical therapy in the management of preterm birth. J Matern Fetal Neonatal Med 2009;22(Suppl 3):72-76. PMID: 19925364.

2. Haas DM, Imperiale TF, Kirkpatrick PR, Klein RW, Zollinger TW, Golichowski AM. Tocolytic therapy: a meta-analysis and decision analysis. Obstet Gynecol 2009;113:585-594. PMID: 19300321.


3. Han S, Crowther CA, Moore V. Magnesium maintenance therapy for preventing preterm birth after threatened preterm labour. Cochrane Database Syst Rev 2013;5:CD000940PMID: 23728634.

4. Diguisto C, Le Ray C, Maillard F, Khoshnood B, Verspyck E, Perrotin F, et al. Individual and organisational determinants associated with maintenance tocolysis in the management of preterm labour: a multilevel analysis. PLoS One 2012;7:e50788PMID: 23272071.



5. Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet 2008;371:75-84. PMID: 18177778.



6. Tucker JM, Goldenberg RL, Davis RO, Copper RL, Winkler CL, Hauth JC. Etiologies of preterm birth in an indigent population: is prevention a logical expectation. Obstet Gynecol 1991;77:343-347. PMID: 1992395.

7. Savitz DA, Blackmore CA, Thorp JM. Epidemiologic characteristics of preterm delivery: etiologic heterogeneity. Am J Obstet Gynecol 1991;164:467-471. PMID: 1992685.


8. Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews TJ, Osterman MJ. Births: final data for 2008. Natl Vital Stat Rep 2010;59:13-71.
9. Romero R, Dey SK, Fisher SJ. Preterm labor: one syndrome, many causes. Science 2014;345:760-765. PMID: 25124429.



10. American College of Obstetricians and Gynecologists. Committee on Practice Bulletins-Obstetrics. ACOG practice bulletin no. 127: management of preterm labor. Obstet Gynecol 2012;119:1308-1317. PMID: 22617615.


11. DeFranco EA, Lewis DF, Odibo AO. Improving the screening accuracy for preterm labor: is the combination of fetal fibronectin and cervical length in symptomatic patients a useful predictor of preterm birth? A systematic review. Am J Obstet Gynecol 2013;208:233.e1-233.e6. PMID: 23246314.


12. Katz M, Goodyear K, Creasy RK. Early signs and symptoms of preterm labor. Am J Obstet Gynecol 1990;162:1150-1153. PMID: 2140235.


13. Copper RL, Goldenberg RL, Davis RO, Cutter GR, DuBard MB, Corliss DK, et al. Warning symptoms, uterine contractions, and cervical examination findings in women at risk of preterm delivery. Am J Obstet Gynecol 1990;162:748-754. PMID: 2316582.


14. Brownfoot FC, Gagliardi DI, Bain E, Middleton P, Crowther CA. Different corticosteroids and regimens for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 2013;8:CD006764PMID: 23990333.

15. Hiersch L, Yogev Y, Domniz N, Meizner I, Bardin R, Melamed N. The role of cervical length in women with threatened preterm labor: is it a valid predictor at any gestational age. Am J Obstet Gynecol 2014;211:532.e1-532.e9. PMID: 24907701.


16. Keskin U, Ulubay M, Kurt YG, Fidan U, Kocyigit YK, Honca T, et al. Increased neopterin level and chitotriosidase activity in pregnant women with threatened preterm labor. J Matern Fetal Neonatal Med 2014;28:1-5. PMID: 24641184.


17. Heng YJ, Pennell CE, Chua HN, Perkins JE, Lye SJ. Whole blood gene expression profile associated with spontaneous preterm birth in women with threatened preterm labor. PLoS One 2014;9:e96901PMID: 24828675.



18. Van Vliet EO, Boormans EM, de Lange TS, Mol BW, Oudijk MA. Preterm labor: current pharmacotherapy options for tocolysis. Expert Opin Pharmacother 2014;15:787-797. PMID: 24533566.


19. Flenady V, Hawley G, Stock OM, Kenyon S, Badawi N. Prophylactic antibiotics for inhibiting preterm labour with intact membranes. Cochrane Database Syst Rev 2013;12:CD000246PMID: 24307518.

Fig. 1
Frequency of hospital admission according to gestational age in women with threatened preterm labor. A trend shows that the number of hospital admission increased in proportion to gestational age.
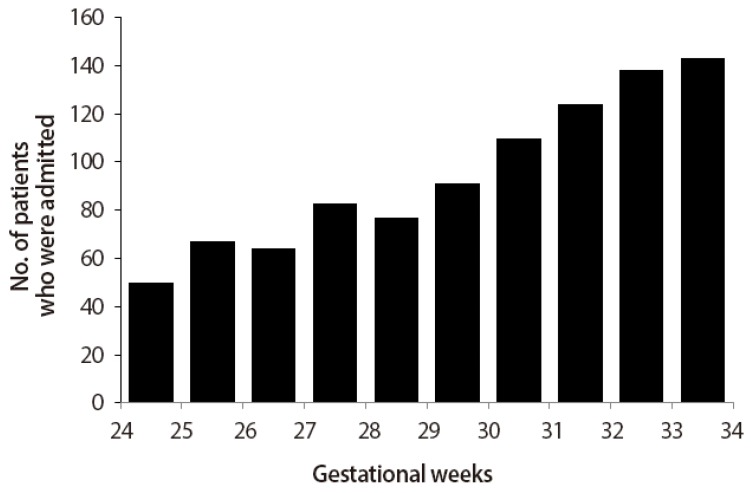
Fig. 2
Betamethasone was more frequently used than the dexamethasone (71.0% vs. 29.0%) (A). The completion rate of betamethasone treatment was higher than that of dexamethasone (B,C).
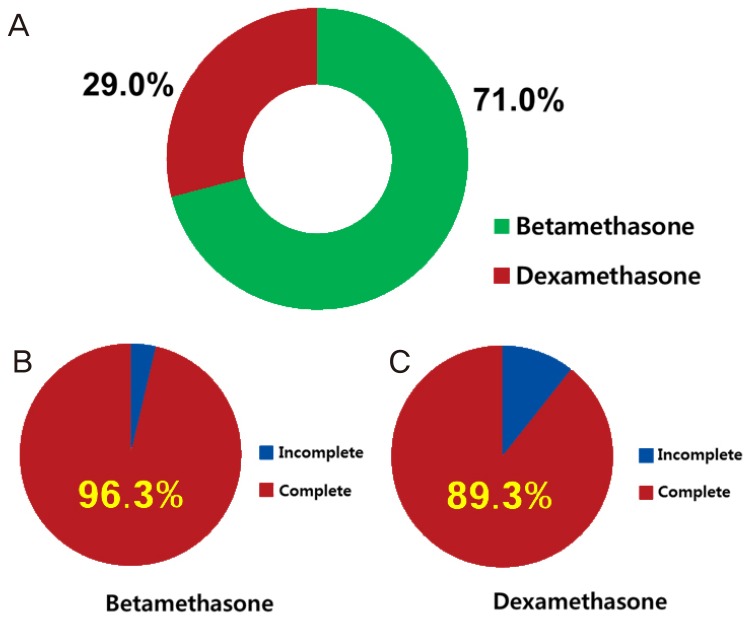
Table 2
Practice pattern and unintended discontinuation of tocolytic therapy in 947 subjects with threatened preterm labor
-
METRICS

-
- 16 Crossref
- 10,092 View
- 52 Download
- Related articles in Obstet Gynecol Sci
-
Dietary pattern and risk of endometrioma in Korean women: a case-control study2021 January;64(1)