|
 |
- Search
| Obstet Gynecol Sci > Volume 65(5); 2022 > Article |
|
Abstract
Objective
Methods
Results
Conclusion
Acknowledgments
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported. Ki Hoon Ahn and Geum-Joon Cho have been an Editorial Board of Obstetrics & Gynecology Science; however, they are not involved in the peer reviewer selection, evaluation, or decision process of this article. Otherwise, no other potential conflicts of interest relevant to this article were reported.
Ethical approval
The KNHANES was approved by the Ethics Committee of the Korea Centers for Disease Control and Prevention (2007-02CON-04-P, 2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C, 2013-07CON-03-4C, and 2013-12EXP-03-5C).
Patient consent
All study participants provided written informed consent to agree with the data to be used in national statistics and research.
Funding information
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2020R1C1C1013579) and the Public Interest Medical Technology Research Project funded by the Ministry of Health and Welfare (MOHW, Korea; grant No. HI21C1560). The funders had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
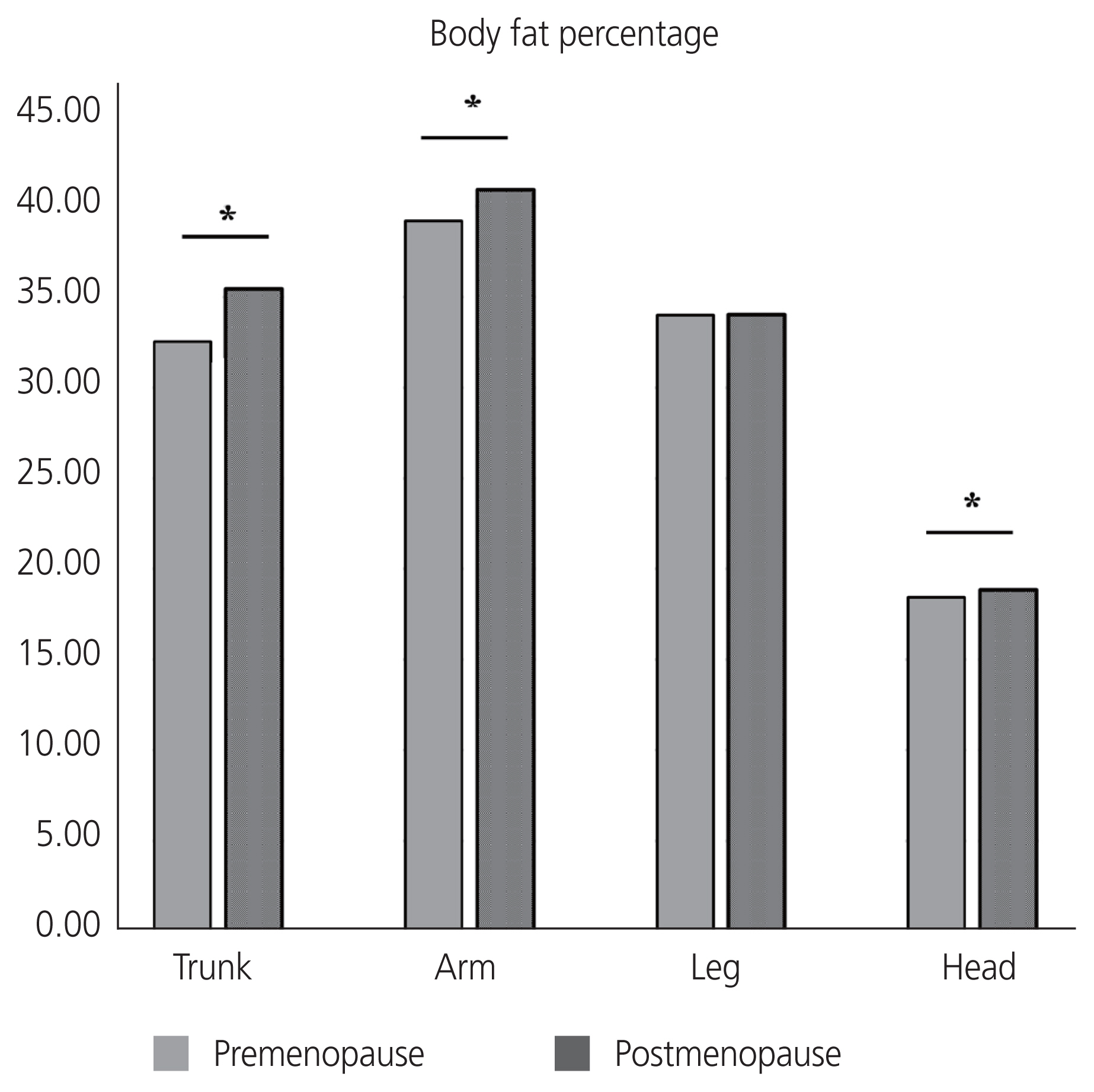
Fig.┬Ā1